Key Points:
- Study looks at potential effects of clot length on acute ischemic stroke patients receiving thrombectomy
- Length not associated with complication risk, outcomes, or number of passes needed
Clot length does not appear to be a relevant clinical factor when selecting patients for thrombectomy for the treatment of acute ischemic stroke. Results of a small retrospective study published online September 15, 2016, ahead of print in the Journal of NeuroInterventional Surgery suggest there is no link between clot length and the risk of complications or poor outcome.
“The recent thrombectomy trials achieved a decent recanalization rate of about 70-90% (TICI 2b-3),” lead author Markus A Möhlenbruch, MD, of Heidelberg University Hospital (Heidelberg, Germany), told Neurovascular Exchange in an email. “The question is why the remaining 10-30% could not be recanalized sufficiently. A retrospective study by Riedel et al. in 2011 has shown that IV thrombolysis with recombinant tPA fails to recanalize occluded vessels with a thrombus length exceeding 8 mm. However, data on the impact of thrombus length on successful mechanical recanalization are sparse.”
To determine the impact of thrombus length, Dr. Möhlenbruch and colleagues retrospectively analyzed angiographic and clinical data from 72 consecutive patients with acute occlusion of the M1 segment of the middle cerebral artery who were treated using stent retrievers.They defined successful recanalization as TIC 2b-3 and a good neurological outcome as mRS ≤ 2 at 90 days after stroke onset.
Thrombus length was distributed normally (P = .211) and was 13.4 ± 5.2 mm (range 3-30 mm). The aforementioned 2011 study “determined a cutoff value of 8 mm for IV thrombolysis,” pointed out Dr. Möhlenbruch. “Therefore, it can be stated that the thrombus sizes measured in our study are representative.”
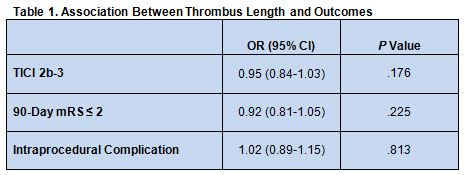
Univariate binary logistic regression analysis did not reveal any association between thrombus length and the likelihood of good clinical outcome or successful recanalization. There was also no association between thrombus length and the risk of intraprocedural complications, including embolization in a new territory (table 1).
The median number of passes needed to achieve recanalization was 2, with no differences based on thrombus length in the number of passes needed. Nor were there differences in atrial fibrillation or use of IV thrombolysis
Other Clot Features May Play a Role
In a telephone interview with Neurovascular Exchange, Charles Prestigiacomo, MD, of Rutgers New Jersey Medical School (Newark, NJ) and president of the Society of NeuroInterventional Surgery, said that this study is the natural progression of research demonstrating that clots larger than 8 mm may not be amenable to IV thrombolysis treatment. “If you’re doing mechanical thrombectomy,” he said, “the length of the clot is not going to be the issue. It may be other parameters.”
Dr. Möhlenbruch credits the design of modern stent retrievers with the high success rates seen in recent thrombectomy trials. Still, he noted, “there are some patients who will probably not benefit from mechanical thrombectomy, [such as] patients with major infarct core, poor collaterals and prolonged time window. . . . Further experimental and clinical studies are necessary to analyze the impact of other factors, [such as] clot composition or density, on recanalization success,”
Source:
Seker F, Pfaff J, Wolf M, et al. Impact of thrombus length on recanalization and clinical outcome following mechanical thrombectomy in acute ischemic stroke. J NeuroIntervent Surg. 2016;Epub ahead of print.
Disclosures:
- Dr. Möhlenbruch reports receiving consulting honoraria, speaker honoraria, and travel support unrelated to this study from Acandis, Codman, Covidien, MicroVention, Phenox, and Stryker.
- Dr. Prestigiacomo reports being a consultant for education to Stryker, Codman, and Aesculap.