Key Points:
- Retrospective study compares two thrombectomy approaches for M2 occlusions
- Stent retrievers linked to faster reperfusion, but forced arterial suction thrombectomy may offer less distal embolization and higher first attempt reperfusion
In M2 occlusions, forced arterial suction thrombectomy (FAST) and stent retriever thrombectomy each have a role to play, a small retrospective study suggests. Operators can make the best choice between them by taking into account the precise location of the lesion and individual anatomy.
The findings were published online July 5, 2016, ahead of print in the Journal of NeuroInterventional Surgery.
Clinical trial data strongly support use of stent retrievers for the treatment of occlusions in the proximal intracranial artery, Yang-Ha Hwang, MD, of Kyungpook National University Hospital (Daegu, South Korea), and colleagues write, but it remains less clear how best to approach occlusions of the distal intracranial artery.
Theoretically, the researchers note, M2 arteries have a smaller ischemic core and ischemic penumbra combined with a thin vessel wall and narrow lumen, potentially putting them at greater risk for complications of endovascular therapy than M1 arteries.
“To date there has been no direct comparison of two frequently used [endovascular thrombectomy] methods (stent retriever and aspiration thrombectomy using a large-bore catheter) in patients with M2 occlusions,” they say.
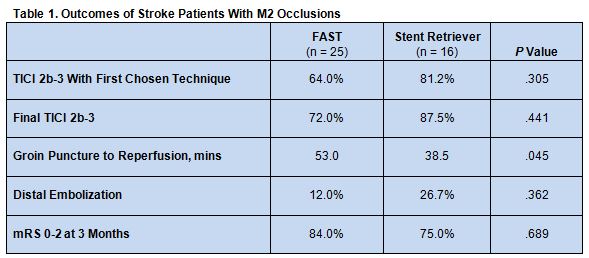
To help clarify which approach is more beneficial, the investigators retrospectively analyzed data on 41 patients with M2 occlusions who were treated with FAST (n = 25) or thrombectomy using a Penumbra stent retriever (n = 16).
There were no differences between the 2 groups of patients with respect to the proportion who achieved a TICI score 2b-3 using the first chosen technique or who achieved a final TICI score of 2b-3. Also similar were rates of distal embolization and final clinical outcome. Time from groin puncture to reperfusion was significantly shorter for the stent retriever thrombectomy group, however (table 1).
Angiographic findings revealed a possible association between the location of the occlusion and the success of FAST. “If the thrombus was located immediately after severe acute angulation,” write the authors, “especially interposition from M1 to M2, it would disturb the optimal contact of the Penumbra catheter tip and the thrombus.” They suggest FAST might be ineffective in such cases because of imprecise facing with the thrombus and catheter tip and that such lesions might be better treated with a stent retriever.
Larger Trials Needed to Confirm Numerical Differences
Given the small sample size of the study, the investigators speculate that some of the numeric but nonstatistically significant differences between the 2 groups may reflect real differences. “Stent retriever thrombectomy may provide faster reperfusion than FAST, while the FAST technique might be associated with lower distal embolization and a higher reperfusion rate for the first thrombectomy attempt, but without any significant difference in clinical outcome,” they write, acknowledging that large, randomized trials are needed for confirmation.
In the meantime, the authors recommend, “When choosing the [endovascular] method for M2 occlusions, consideration of the location of the occlusion and tortuosity between M1 and M2 might be helpful to achieve a better angiographic outcome.”
Source:
Kim YW, Son S, Kang DH, et al. Endovascular thrombectomy for M2 occlusions: comparison between forced arterial suction thrombectomy and stent retriever thrombectomy. J NeuroInterv Surg. 2016;Epub ahead of print.
Disclosures:
Dr. Hwang reports no relevant conflicts of interest.