Key Points:
- Study compares outcomes of mechanical thrombectomy with, without bridging thrombolysis among eligible patients
- Outcomes similar apart from higher bleeding, mortality risks with bridging
Direct, rapid mechanical thrombectomy for the treatment of large anterior circulation stroke may produce outcomes as good as those achieved with the addition of bridging thrombolysis, even among patients who were eligible for bridging. The findings, from a retrospective analysis, were published in the April 2016 issue of Stroke.
Using data from the Bernese stroke registry, Urs Fischer, MD, of the University of Bern, Inselspital, Freiburgstrasse (Bern, Switzerland), and colleagues reviewed clinical and radiological outcomes of patients with large artery anterior circulation stroke: 167 received bridging thrombolysis prior to intervention and 255 received direct mechanical thrombectomy using aspiration or a stent retriever. All patients from nonbridging group who would have qualified for IV tissue plasminogen activator (tPA) were matched, using multivariate and propensity score analyses, with controls from the bridging group.
Between February 2009 and August 2014, 40 patients from the direct mechanical thrombectomy group would have qualified for bridging thrombolysis but were treated with mechanical thrombectomy only. These patients did not differ from matched bridging patients with respect to clinical or radiological characteristics, with the exception of having higher rates of hypercholesterolemia (P = .019) and coronary heart disease (P = .039) as well as shorter intervals from symptom onset to endovascular intervention (P = .01).
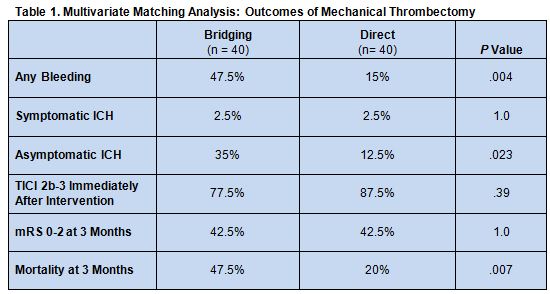
In the adjusted and matched analysis, the rates of complete reperfusion (TICI 2b-3) immediately after intervention, symptomatic intracerebral hemorrhage (ICH), and 3-month functional independence (mRS score 0-2) did not differ between the 2 groups. However, rates of any bleeding, asymptomatic ICH, and 3-month mortality all were higher in the bridging patients (table 1)
In an email to WLNCMD, Perry Ng, MD, of Centura Health Physician Group (Denver, CO), explained that while mechanical thrombectomy in conjunction with IV tPA is standard of care for large vessel occlusion in most centers, patients often miss the time window for this therapy or have contraindications to it, so it is not uncommon for patients to go without. IV tPA can be particularly helpful, he noted, when endovascular therapy is unavailable or if patients must be transferred long distances to receive it.
“This study implies that in patients with large vessel occlusion presenting early (within the time window for IV tPA) and likely at or near a stroke facility capable of endovascular therapy, where it can be offered expeditiously (median time 4.37 hours in this study), there is no difference in clinical outcomes at 90 days,” said Dr. Ng. “Moreover, there may be a safety benefit, including lower mortality and asymptomatic ICH rates in patients treated with endovascular therapy alone. However, the cause of the higher mortality in the bridging group is not given, and the symptomatic ICH rate is not increased, so whether the higher mortality is due to the bridging therapy or unrelated cause is unclear.”
Other limitations of the study, noted Dr. Ng, include its small sample size, retrospective nature, and lack of important clinical details.
“The reason why certain patients were not bridged with IV tPA and others were is not well documented. Hence, selection bias could be a factor limiting the generalizability of the results,” he said. “There is also a lack of details as to which endovascular devices were used, the number of passes required to achieve recanalization, and the frequency of intra-arterial thrombolytic (urokinase) administration in each subgroup. In addition, an unknown number of patients in the bridging group were treated with a lower dose of IV tPA (0.6mg/kg) instead of the standard dose (0.9mg/kg) for unstated reasons.”
Because of these drawbacks, said Dr. Ng, a prospective randomized trial is needed to confirm the results. It is possible that, if confirmed, “dispensing with IV tPA bridging therapy in a subset of patients where endovascular therapy is readily available would potentially save time and allow endovascular therapy to be started earlier as well as save the cost of the tPA medication,” he commented. The study authors write that they have planned just such a trial.
The findings of this study dovetail with those of a recent trial by Rebello et al. In that study, outcomes were also compared between patients who did and did not receive IV tPA prior to endovascular stroke therapy, but patients in that study who did not receive bridging were in fact ineligible for it. Rates of reperfusion and good outcome were found to be similar for both groups.
Taken together, the two retrospective studies bolster the case for direct mechanical thrombectomy in patients who are treated early and are without extensive brain infarction (ASPECTS ≤ 6), said Dr. Ng.
Source:
- Broeg-Morvay A, Mordasini P, Bernasconi C, et al. Direct mechanical intervention versus combined intravenous and mechanical intervention in large artery anterior circulation stroke: A matched-pairs analysis. Stroke. 2016;47:1037-1044.
Disclosures:
- Dr. Fischer reports receiving Speakers honoraria for Covidien and serving as a consultant to Medtronic.
- Dr. Ng reports no relevant conflicts of interest.