Key Points:
- Registry study looks at 109 patients with acute infarction limited to vascular territory of 1 ICA, no large-vessel atherosclerosis
- Intraplaque high-intensity signal on MRA linked to strokes of unknown etiology
Using standard imaging techniques to identify large-artery lesions containing intraplaque hemorrhage could help clinicians better understand stroke cases that would otherwise be labeled as cryptogenic, according to research presented on February 17 at the 2016 International Stroke Conference in Los Angeles, CA.
The findings also were published online ahead of print in JACC: Cardiovascular Imaging.
Ajay Gupta, MD, of Weill Cornell Medical College (New York, NY), and colleagues examined the association between non-stenosing, vulnerable large-artery plaque and ischemic stroke using data from their prospective stroke registry. They identified 109 patients with acute infarction limited to the vascular territory of one internal carotid artery (ICA) and no large-vessel atherosclerosis, based on the criterion of ≥ 50% luminal stenosis.
“All brain MRI and neck [magnetic resonance angiography (MRA)] studies were performed using standard MRI equipment without high-resolution surface carotid coils or gadolinium,” the authors write. “We ascertained complicated carotid plaque based on the qualitative assessment of intraplaque high-intensity signal (IHIS) on axial 3D-time-of-flight images, a presumed marker for intraplaque hemorrhage.
In an email correspondence with WLNCMD, Dr. Gupta explained that, “we intentionally designed our study to leverage MRI technology to study plaque that can be implemented without specialized hardware, contrast agents, or pulse sequences that are not commercially available.”
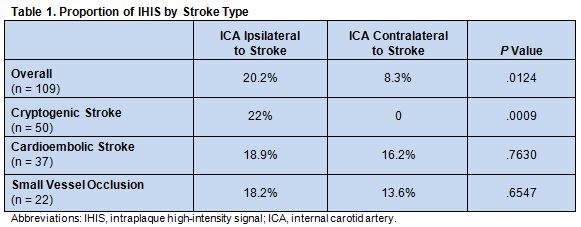
The investigators studied 218 arteries in 109 patients. Of these, 31 (14.2%) contained vulnerable ICA plaque, defined as having IHIS on MRA. Among the 31 IHIS-positive lesions, 22 occurred ipsilateral to the side of the patient’s infarction and 9 occurred contralateral to the side of infarction (P = .01). When stratified by stroke subtype, IHIS was associated with infarctions that were classified as being of unknown etiology (ie, cryptogenic) but not with those due to cardioembolism or small-vessel occlusion (table 1).
“Currently, nearly 1 in 3 strokes has no clear cause,” noted Dr. Gupta. “We believe that atherosclerosis of the ICA, which has historically been unrecognized (or even ignored) because it does not cause ≥ 50% stenosis of the carotid artery, may be a cause of a significant proportion of these cryptogenic strokes. Using the MRI techniques proposed in this study, we found that these high-risk plaques (containing intraplaque hemorrhage) tend to occur on the same side of these cryptogenic strokes suggesting that such nonstenosing plaques may be the cause.”
“Our next step would be to confirm our study in a large prospective observational study of patients with strokes of undetermined etiology,” he continued. The focus would be on stroke recurrence, since the researchers hypothesize that patients with nonstenosing high-risk ICA plaque are at relatively high risk of repeat events.
Jaget Narula, MD, PhD, of Mount Sinai St. Luke’s and Mount Sinai West (New York, NY), told WLNCMD in an email that the study has “a very well-conceived design for evaluating the strokes hitherto considered cryptogenic.”
Intraplaque hemorrhage, he added, is a high-risk feature known to be frequently associated with stroke, is well validated in stenotic plaques, and can be easily obtained using rapid standard acute stroke imaging protocols. “Knowing plaque composition should allow for targeted or personalized therapy and result in reduction of stroke recurrences,” Narula said, echoing the sentiment that larger, prospective trials are needed to confirm the findings.
Source:
Gupta A, Gialdini G, Giambrone AE, et al. Association between non-stenosing carotid artery plaque on magnetic resonance angiography and acute ischemic stroke. J Am Coll Cardiol Img. 2016;Epub ahead of print.
Disclosures:
- Drs. Gupta and Narula report no relevant conflicts of interest