Key Points:
- Two studies look at how hospitals employ new stroke protocols
- Both achieve shorter door-to-needle times, while one hospital had improved outcomes
Two hospitals, one located in a rural setting and another in a dense urban area, have developed protocols that significantly reduced door-to-needle time for the endovascular treatment of patients presenting with large occlusion strokes. The protocols they developed can likely help other hospitals do the same, researchers say.
Both studies are published online ahead of print earlier this month in the Journal of NeuroInterventional Surgery.
For one study, led by Dr. Johanna T Fifi, MD, of the Icahn School of Medicine at Mount Sinai (New York, NY), researchers conducted a retrospective review of 69 patients with ischemic stroke treated with intra-arterial therapy. Cohort 1 (n = 32) included patients treated before implementation of a new acute stroke protocol developed to improve efficiencies, and cohort 2 (n = 37) included patients treated after its adoption.
“Before this time, acute strokes were handled in a non-standardized fashion that depended upon the on-call neurology or interventional physician attending, with informal and variable interdepartmental communication,” paper explains. Key features of the new approach included:
- Empowerment of the triage nurse to call a stroke code and mandate that the stroke team be notified when prenotification was provided to the ED by emergency medical services
- Automatic acquisition of CTA of the head and neck in patients arriving within 6 hours of symptom onset
- Extension of the period of notification to 6 hours from last known well or symptom discovery for wake-up strokes
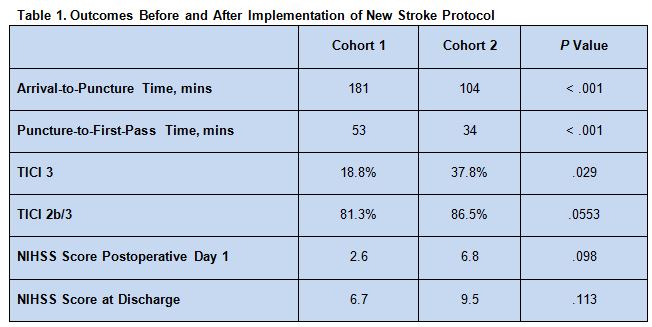
Patients treated after the implementation of the protocol had a decreased arrival-to-puncture time and puncture-to-first-pass time and were more likely to have a Thrombolysis in Cerebral Infarction (TICI) score of 3. There also were trends toward more patients in the second cohort having a TICI of 2b/3 and a higher National Institute of Stroke Scale (NIHSS) score on postoperative day 1 and at discharge (table 1).
The 2 groups did not differ with respect to modified Rankin Scale score at discharge, though there was a slight trend toward better function in the second cohort of patients. Rates also were similar for symptomatic intracerebral hemorrhage (10.8% vs. 9.4%, P = 0.957) and death (10.8% vs. 15.6%, P = 0.553).
Six Sigma Approach to QI
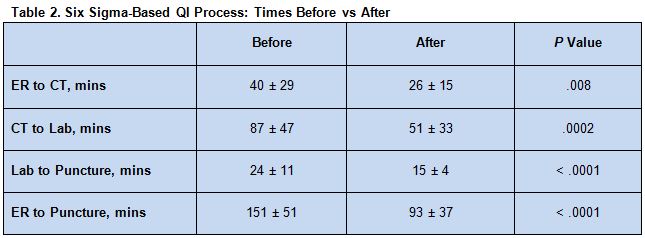
The other study, by Ansaar T Rai, MD, of West Virginia University (Morgantown, WV), and colleagues, looked at the effects of a Six Sigma-based Quality Improvement (QI) process developed over 3 months. The program aimed to identify and address rate-limiting steps in the endovascular care pathway. Rai et al prospectively recorded treatment times and then compared them among 64 patients treated before the changes and 30 patients treated afterward.
Implementation of the QI protocol was associated with significantly shortened durations for all 3 time intervals assessed (table 2).
The improved times were seen for both working-hours and off-hours interventions.
This study did not evaluate outcomes. In a telephone interview with WLNCMD, Dr. Rai explained why: “Our hypothesis is that [better timing] will improve outcomes. The reason we did not report outcomes specifically is we did not want to get sidetracked into conversation of which device is better.” Also, there was some heterogeneity between the 2 groups with respect to how the procedure was performed, as surgical protocols also changed over time. Their goal is to eventually report outcomes in a larger pool of patients, he said.
Going Above and Beyond Recent Trials
The impetus to improve treatment times is a direct result of recent clinical trials demonstrating the benefits of intra-arterial therapy for large occlusion strokes, Dr. Fifi told WLNCMD in a telephone interview. “Now we know this is an effective therapy, it’s become standard of care, and we all know time is brain, so there is no point in doing the procedure unless you’re doing it quickly and efficiently.”
Taken together, the studies provide important insight into how individual hospitals in various settings can make changes that are appropriate to them, Dr. Rai said, noting that his study took place at a rural center while that of Fifi et al took place at hospital located in an urban setting.
Jeannie Pittenger, RN, a stroke program facilitator at HSHS Sacred Heart Hospital (Eau Claire, WI), told WLNCMD that studies such as these provide practical insight for hospitals aiming to improve their door-to-needle time. Not only do they provide a number of options for systems improvement that hospitals can pick and choose from depending on their needs, but they provide the hard evidence required to get clinical staff on-board with changes. Another crucial step to developing a successful new workflow protocol, she said, is ensuring that the end-users—the emergency room staff, radiology department, and clinical stroke faculty—are involved in its development.
Dr. Fifi said she believes that even more can be done to reduce the time from symptom onset to puncture, but it is necessary to look beyond what happens at a single hospital. “We have a lot of patients who are transferred in from other hospitals, and that’s a big black hole when it comes to losing time,” she stressed. “If you present to a hospital that doesn’t have [interventional radiology] capabilities, and you have to be transferred out of that hospital into a different setting, that can take a couple of hours.”
Solutions to that problem, she said, will vary considerably by region, depending on the location of the nearest comprehensive stroke center in relation to the nearest primary stroke center, the ability of emergency medical services to identify large occlusion strokes, and the ability and willingness of competing health systems to work together.
“What’s important is that people know that it can be done,” she said. “Eventually, these timing goals may become part of accreditation, so maybe that will be the impetus to get more people to start doing it.”
Sources:
1. Mascitelli JR, Wilson N, Shoirah H, et al. The impact of evidence: evolving therapy for acute ischemic stroke in a large healthcare system. J NeuroInterv Surg. 2016;Epub ahead of print.
2. Rai AT, Smith MS, Boo S, et al. The ‘pit-crew’ model for improving door-to-needle times in endovascular stroke therapy: A Six-Sigma project. J NeuroInterv Surg. 2016;Epub ahead of print.
Disclosures:
- Drs. Rai and Fifi and Ms. Pittenger report no relevant conflicts of interest.