Key Points:
- Researchers assesses impact of severe hypoperfusion on outcomes after endovascular therapy
- No increased risk of intracranial hemorrhage, disability, or death with severe hypoperfusion
Severe hypoperfusion among patients with acute ischemic stroke does not heighten the risk of intracranial hemorrhage or other negative outcomes following endovascular treatment that results in full reperfusion.
For their paper published online November 24, 2015, ahead of print in Stroke, Raul G. Nogueira, MD, of Emory University and Grady Memorial Hospital (Atlanta, GA), and colleagues performed a retrospective database review of 113 cases of endovascular therapy for acute ischemic stroke between September 2010 and March 2015.
All patients included in the study had anterior circulation occlusions, with baseline CT perfusion determined using RAPID software (iSchemaView; Menlo Park, CA). They all achieved full reperfusion, defined as a modified Thrombolysis in Cerebral Infarction (mTICI) score of 3.
Overall, 37 patients had severe hypoperfusion (Tmax > 10 s > 100 mL on CT perfusion). Theyhad higher baseline National Institutes of Health Stroke Scale (NIHSS) scores (20.7 ± 3.8 vs. 17.0 ± 5.9, P < 0.01), more internal carotid artery terminus occlusions (29% vs. 9%, P = 0.02), and larger infarct volumes at baseline (38.6 ± 29.6 vs. 11.7±15.8 mL, P < 0.01) and after treatment (60.7 ± 60.0 vs. 29.4 ± 33.9 mL, P < 0.01) than did the 76 patients without severe hypoperfusion. Otherwise, the 2 groups were comparable.
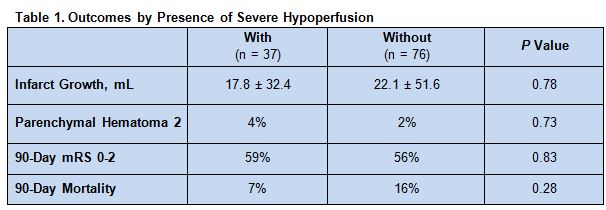
After treatment, there were no statistically significant differences in infarct growth or in the rates of severe intracranial hemorrhage, good outcomes at 90 days, or mortality at 90 days between patients with and without severe hypoperfusion (table 1).
On multivariate analysis, only baseline NIHSS score (OR 1.19, 95% CI1.06-1.34, P < 0.01) and baseline infarct core volume (OR 1.05, 95% CI 1.02-1.08, P < 0.01) were independently associated with the presence of severe hypoperfusion. There were no links between severe hypoperfusion and intracranial hemorrhage, good outcome, or infarct growth.
Optimizing Patient Selection
“In the setting of limited baseline ischemic cores, large Tmax>10 s lesion volumes on CT perfusion do not seem to be associated with a higher risk of clinically relevant [intracranial hemorrhage] and does not preclude good outcomes in patients achieving successful endovascular reperfusion with the contemporary technology,” write the authors. “Thus large Tmax>10 s penumbral lesion volumes in isolation should not be used to exclude patients from endovascular therapy.”
However, whether these conclusions extend to patients selected with MRI perfusion must be determined by future studies, they stress.
“Our findings are of substantial importance,” Dr. Nogueira and colleages say. “As the rates of optimal reperfusion (mTICI 2b-3) are now in the 70% to 90% range, optimizing patient selection became increasingly important in the quest to further improve patient outcomes.
Yet selection techniques should not be used to reject candidates who might still potentially benefit from reperfusion, they urge, citing the SWIFT Prime trial which excluded CT perfusion-selected patients with severe hypotension.
Source:
Nogueira RG, Haussen DC, Dehkharghani S, et al. Large volumes of critically hypoperfused penumbral tissue do not preclude good outcomes after complete endovascular reperfusion: Redefining malignant profile. Stroke. 2016;Epub ahead of print.
Disclosures:
- Dr. Nogueira served as the PI for the Trevo-2 and DAWN trials (Stryker-Neurovascular), was on the steering committee for the SWIFT and SWIFT-PRIME trials (Covidien), part of the core laboratory for the STAR trial (Covidien), and on the executive committee for the 3-D Separator trial (Penumbra).