Key Points:
- Study models cost-effectiveness of endovascular therapy on top of standard care alone for LVO
- Addition of endovascular stroke therapy cost-effective for most patients
Wolfgang G. Kunz, MD, of LMU Munich (Munich, Germany) and colleagues used a decision model based on Markov simulations to estimate lifetime costs and quality-adjusted life years (QALYs) of stroke therapy over 30 years in 1-year cycles. During each cycle, patients could remain in the same health state, experience a recurrent stroke and recover to the same mRS, transition to a lower mRS, or die from other causes.
Data inputted into the model were obtained from recently published literature including 5 randomized controlled trials: ESCAPE, EXTEND-IA, MR CLEAN, REVASCAT, and SWIFT PRIME. The investigators also conducted probabilistic sensitivity analysis to estimate the uncertainty of the model results. Willingness-to-pay was set to $50,000/QALY.
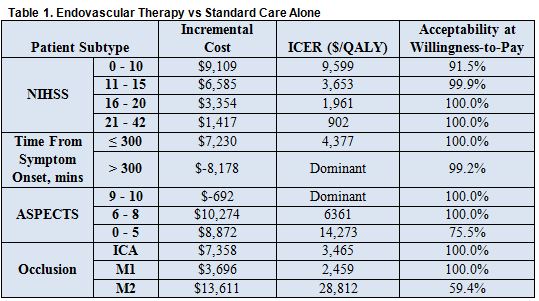
Overall, endovascular therapy with standard care was found to be more cost-effective than standard care alone. The addition of endovascular therapy led to increased QALYs in all patient subgroups, and mean incremental cost-effectiveness ratios (ICERs) were considered acceptable. Results were equivocal only in patients with ASPECTS ≤ 5 or M2 occlusions, as these patients had much higher ICERs and only reached suboptimal acceptability in the probabilistic sensitivity analysis (table 1).
In an email to Neurovascular Exchange, Dr. Kunz stood strongly behind his results. “Decision analytic models are designed to incorporate as much of available evidence to simulate the implied costs and effectiveness of diagnostic or treatment strategies,” he explained. “Due to the comparability of the overall results in [other] studies, which used slightly different approaches and country-specific model input parameters, we conclude that the results are reliable.”
He pointed out that these findings likely apply to multiple different healthcare settings, since previous studies set in different countries have yielded similar results. These include other studies in the United States, 2 in the United Kingdom (found here and here), 1 in Canada, and another in Sweden.
But “transferability of cost-effectiveness evaluations onto other healthcare systems should be regarded with caution as there can be considerable differences, in particular regarding the implied treatment costs,” he warned.
“The novelty of our study is the analysis of patient subgroups with acute ischemic stroke who are eligible for endovascular therapy,” explained Dr. Kunz. “This was enabled by a recent meta-analysis of 5 large randomized controlled trials. In particular, the results in the subgroup of patients presenting more than 5 hours after symptom onset are interesting. Although the combined treatment effect is smaller compared to patients presenting earlier, this approach saved healthcare costs in the long run despite the fact that the initial expenditures are higher.”
Altogether, he concluded “these results provide evidence to invest in the healthcare infrastructure in order to provide around-the-clock and nationwide accessibility to endovascular stroke therapy for patients.” As future studies are performed and further technological advances occur, cost-effectiveness should be re-evaluated, Dr. Kunz advised.
Source:
- Kunz, WG, Hunink MGM, Sommer WH, et al. Cost-effectiveness of endovascular stroke therapy: a patient subgroup analysis from a US healthcare perspective. Stroke. 2016;Epub ahead of print.
Disclosures:
- Dr. Kunz reports no relevant conflicts of interest.