Key Points:
- Study examines outcomes of endovascular therapy for LVO involving minimal symptoms
- Greater improvement in NIHSS score with endovascular vs medical therapy
There is a potential role for endovascular intervention among patients with large vessel occlusions (LVOs) who present with minimal symptoms, according to research published online September 2, 2016, ahead of print in the Journal of NeuroInterventional Surgery.
The decision to treat patients with medical therapy (n = 22) or endovascular intervention (n = 10) was made after careful discussion with patients and their families. Signs of deterioration, which included development of aphasia, neglect, and/or significant weakness, triggered reconsideration of thrombectomy.
The question of whether strokes with minimal symptoms should be treated endovascularly remains controversial, Haussen and senior author Raul G. Nogueira, MD, also of Grady Memorial, told Neurovascular Exchange in a joint email.
“A similar debate about whether intravenous thrombolysis should be performed for patients with mild symptoms has existed for the past several years,” they noted. “Large cohort studies have demonstrated that approximately 30% of the patients presenting with so-called mild strokes (eg, NIHSS ≤ 5) may end up having significant disability.”
“Thrombectomy for mild stroke presentations is relatively uncommon but not rare,” Haussen and Nogueira continued. “Our entire cohort of patients with minimal clinical severity who underwent thrombectomy (including the ones who were treated after deterioration) represented < 5% of our total volume of stroke interventions. Importantly, it is very likely that patients with mild stroke presentations and underlying large vessel occlusion are underrecognized and/or not referred for endovascular consultation.”
Baseline characteristics between the patients treated with thrombectomy and those were treated with medical therapy were comparable. Among the 22 patients initially treated with medical therapy, 9 (41%) experienced subsequent deterioration requiring thrombectomy. The median time from arrival to deterioration was 5.2 hours ( range, 2.0-25.0).
Successful reperfusion, defined as a modified TICI 2b-3, was achieved in all 19 thrombectomy patients.
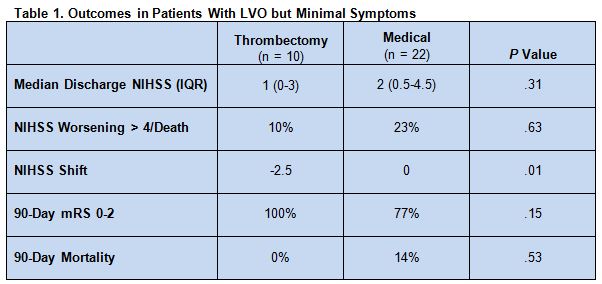
The change in NIHSS score from admission to discharge significantly favored thrombectomy. Median NIHSS score at discharge was low for both thrombectomy and medical therapy (table 1).
Multivariable linear regression revealed that thrombectomy was independently associated with a beneficial NIHSS shift (unstandardized β -4.2, 95% CI -8.2 to -0.1, P = .04).
Good Safety, Better Outcomes With Thrombectomy
“Intuitively, endovascular intervention for patients with mild stroke presentation could be perceived by many as less appealing, considering its higher degree of invasiveness, inherent risks, and expenses,” the authors told Neurovascular Exchange. “However, patients with LVO are thought to more often suffer clinical deterioration as compared to patients with mild symptoms without underlying LVO.”
Importantly, the study results “not only showed a significant chance of deterioration with conservative therapy but also suggested that intervention could be performed with an acceptable degree of safety in these patients and seemed to lead to better outcomes,” they said. While there are risks associated with an endovascular approach, the researchers acknowledged, “we believe that the risks of vessel damage and reperfusion hemorrhage for patients with mild symptoms should be similar or lower . . . when compared to patients with more severe presentations.”
According to Charles Prestigiacomo, MD, of Rutgers New Jersey Medical School (Newark, NJ) and president of the Society of NeuroInterventional Surgery, now that studies have demonstrated the benefits of endovascular interventions for ischemic stroke, the next step is to identify those patients most likely to benefit from such treatment.
“It was interesting that the patients who did worse were the ones who had deterioration that occurred more than 3 hours after,” he said. “What that tells me is we need to better study the collateral circulation.”
The authors agree. “Based on clinical experience,” they said, “we only we consider the following patients as potentially having higher risk for subsequent deterioration: 1) patients who earlier in their presentation had a higher NIHSS; 2) patients who are auto-hypertensing as they . . . may not be able to sustain that for a long time; 3) patients who show exam deterioration upon going from a supine evaluation to a sitting up evaluation; and 4) patients with imaging patterns characteristic of suboptimal collateral flow on perfusion imaging (eg, significant Tmax or MTT prolongation) or nonrobust collaterals on CT angiography/MR angiography imaging.”
But Dr. Prestigiacomo said that some issues limit interpretation of the study. “It wasn’t clear if they were aggressive about maintaining and controlling blood pressure in those patients who did not go to endovascular treatment,” he pointed out, noting that there could be some people who refused all treatment. “Some of them might potentially have qualified for IV tPA, and that may or may not have helped them,” he said. “We don’t know.”
Dr. Prestigiacomo suggested that national or global registry trials could be a convenient and cost-effective way to further inform patient selection.
Source:
Haussen DC, Bouslama M, Grossberg JA, et al. Too good to intervene? Thrombectomy for large vessel occlusion strokes with minimal symptoms: An intention-to-treat analysis. J NeuroInterv Surg. 2016;Epub ahead of print.
Disclosures:
- Dr. Nogueira reports receiving research funding from Stryker, Covidien, and Penumbra
- Dr. Prestigiacomo reports being a consultant for education to Stryker, Codman, and Aesculap.