Key Points:
- Study assesses hospital’s effort to reduce treatment delays for stroke patients
- Door-to-puncture times significantly reduced but outcomes unchanged
Using 6 widely applicable strategies, experts at the University of Pittsburgh Medical Center (UPMC) have shaved more than 30 minutes off of their median door-to-puncture time for stroke patients.
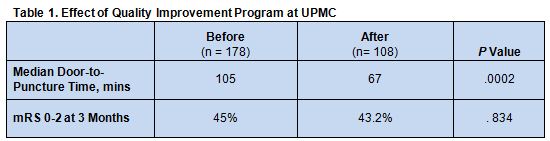
In a paper published online April 5, 2016, ahead of print in the Journal of NeuroInterventional Surgery, Ashutosh P Jadhav, MD, of the UPMC Stroke Institute (Pittsburgh, PA), and colleagues analyzed the effect of a quality improvement program implemented at their center in October 2013. They compared door-to-groin puncture times between 178 patients who were treated before (April 20, 2012-October 8, 2013) and 108 patients treated after (October 9, 2013-July 29 2014).
The main ingredients for optimization were:
- Continuous feedback
- Standardized immediate emergency department (ED) attending to stroke attending
- Communication with interventional team activation for all potential interventions
- Prenotification by emergency medical service (EMS) to minimize additional diagnostic testing
- Direct transport by EMS to the CT scanner
- Direct transport from the CT scanner to the angiography suite
Baseline characteristics were similar for both groups, with the exception of a higher median Alberta Stroke Program Early CT Score (ASPECTS) in the pre-optimization group (P = 0.01).
Door-to-puncture times were lower after implementation of the optimization steps. This did not translate into better functional outcomes at 3 months, however (table 1).
A subgroup analysis of patients with anterior circulation occlusions who received IV tissue plasminogen activator (tPA) revealed a nonsignificant trend toward better outcomes postoptimization, after controlling for pretreatment ASPECT score and National Institutes of Health Stoke Scale score (46.7% vs 51.7%, OR 1.33, 95% CI 0.43-4.16).
Communication, Cooperation Among Staff and Facilities Crucial
In a telephone interview with WLNCMD, Dr. Jadhav explained that stroke centers have yet to develop a centralized system for sharing strategies to minimize treatment delays, so it is difficult to determine how widely used these optimization strategies are. It remains well recognized in the stroke community, however, that faster treatment means better outcomes, so avoiding treatment delays remains a universal priority. The authors attribute the lack of significant differences in outcome between the 2 groups in this study to the small sample size and confounding baseline characteristics.
In addition, said Dr. Jadhav, many treatments for stroke are time-sensitive, so streamlining stroke patients’ evaluation and treatment pathway helps widen the pool of patients eligible for the therapies that are known to be most effective.
There are 3 hospitals within UPMC, and Dr. Jadhav noted that they differ somewhat in their ability to adopt the protocols evaluated for this study.
Many time-saving strategies can be adopted virtually universally, however. Retraining ED personnel so that suspected stroke patients bypass standard triage and go directly to CT scanning is one such strategy, he said. Another is to streamline interfacility communication so that suspected stroke patients are brought immediately to centers with the technology needed to treat them or are rapidly identified for immediate transfer. Imaging data should also be immediately made available to the transfer hospital so that patients can bypass the ED at the incoming hospital altogether. Finally, efforts should be made to ensure that teams work in parallel rather than in sequence and avoid any unnecessary steps, such as Foley catheterization for patients and telephone chains among staff.
One of the most important interventions, said Dr. Jadhav, is simply to start timing processes. This helps staff members recognize where the bottlenecks occur and work toward resolving them.
Minimizing delays does require resource investment, Dr. Jadhav noted, because it means an on-call team must be available at all times and occasional false alarms (a rate he estimates to be at about 15%) are unavoidable.
In a telephone interview with WLNCMD, Jeannie Pittenger, RN, stroke program facilitator at HSHS Sacred Heart Hospital (Eau Claire, WI), agreed that this study offers several useful strategies that have wide applicability. Her center, where metrics surrounding timing of stroke patient care are continuously measured and analyzed at multiple key steps along the treatment pathway, has already adopted many of the strategies evaluated here.
Ms. Pittenger noted that the retraining of ED personnel has proven to be one of the most important and challenging steps. Many standard procedures for evaluating patients in the ED simply do not apply to suspected stroke patients, for whom rapid care is such an important factor, she said In fact, training and retraining of all staff, particularly new staff, is essential to minimizing treatment delays.
Source:
- Aghaebrahim A, Streib C, Rangaraju S, et al. Streamlining door to recanalization processes in endovascular stroke therapy. J NeuroInterv Surg. 2016;Epub ahead of print.
Disclosures:
- Dr. Jadhav and Ms. Pittenger report no relevant conflicts of interest.