Key Points:
- Study looks at endovascular stroke therapy for patients admitted during working vs off-hours
- No impact of admission times on outcomes detected in this single-center study
Regardless of whether stroke patients given endovascular therapy are admitted during hospital working hours or off-hours, their characteristics, procedure times, and clinical outcomes all are similar. The findings, from a single-center German study, were published online March 18, 2016, ahead of print in the Journal of NeuroInterventional Surgery.
Omid Nikoubashman, MD, of University Hospital Aachen (Aachen, Germany), and colleagues identified 6,412 consecutive patients who presented between February 2010 and January 2015 with symptoms of acute ischemic stroke and were evaluated for endovascular treatment.
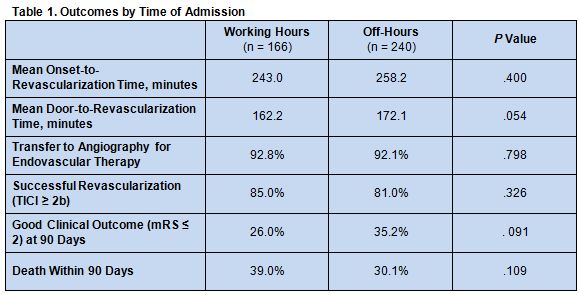
Overall, 410 patients were deemed eligible for endovascular therapy, and 406 accepted the treatment. Of Among these patients, 166 were admitted during hospital working hours (8am to 5pm, Monday thru Friday), and 240 were admitted during off-hours.
Clinical and radiological features did not differ significantly by patients’ admission time. Procedural times, rate of transfer to angiography for endovascular therapy, the likelihood of successful revascularization, and clinical outcomes were all similar for both groups as well (table 1).
In addition, the rationale not to treat patients who were eligible for endovascular therapy did not differ between working-hours and out-of-hours admission (P = .756).
Findings May Not Apply to Other Centers
The authors conclude: “It is possible to establish state-of-the-art reperfusion treatment for [large vessel occlusion acute ischemic stroke] without procedural times and clinical outcome being negatively influenced by time of admission. Our data do not support the hypothesis that treatment decisions are affected by an implicit bias of admission time.”
However, the findings may not be applicable to hospitals with different procedures and protocols, they say, such as those that have vastly reduced staffing during off-hours. In addition, only patients who received reperfusion were prospectively entered into the registry. To identify patients who were admitted for reperfusion therapy but did not receive it, the researchers had to search the database and evaluate patients’ eligibility for reperfusion retrospectively.
As a result of these limitations, the authors acknowledge, prospective studies are needed to confirm their findings.
Source:
- Nikoubashman O, Probst T, Schürmann K, et al. Weekend effect in endovascular stroke treatment: do treatment decisions, procedural times, and outcome depend on time of admission? J NeuroInterv Surg. 2016;Epub ahead of print.
Disclosures:
- Dr. Nikoubashman reports no relevant conflicts of interest