Key Points:
- Evaluation of new imaging protocol, CT stroke study, for assessment of ischemic stroke
- Protocol safe, feasible, with low risk of acute kidney injury
A CT stroke study (CTSS), consisting of a non-contrast CT scan of the brain, a CT perfusion study (CTP) of the head, and CT angiography (CTA) of the head and neck, is a safe and feasible way of evaluating the cerebrovascular axis in patients with symptoms of acute ischemic stroke, according to a study published online February 4, 2016 ahead of print in the Journal of Neurointervention Surgery.
“In the routine diagnosis and treatment of acute ischemic stroke, basic imaging of the brain and cerebrovasculature has become common practice,” write the authors, led by Adnan H Siddiqui, MD, of University at Buffalo Neurosurgery (Buffalo, NY). “Although rapid and effective, iodinated contrast-enhanced CT imaging is not without risk, the primary of which is renal injury. This may be of particular concern in patients who are elderly, diabetic, and those with baseline renal dysfunction.”
Dr. Siddiqui and colleagues assessed the incidence of acute kidney injury (AKI) in 84 patients who underwent a CTSS and digital subtraction angiography (DSA) for evaluation of acute ischemic symptoms or for stroke intervention within a 48 h period between August 2012 and December 2014.
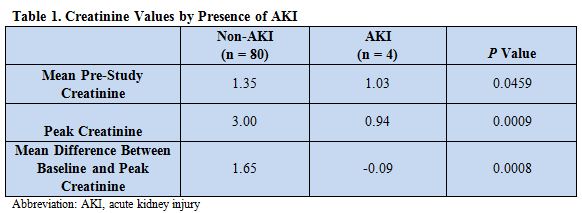
Patients were divided into one of two cohorts: AKI (n = 4), defined as a rise in the serum creatinine level of ≥ 0.5 mg/dL from baseline, or non-AKI (n = 80). One of the patients with AKI had baseline renal dysfunction, defined as baseline serum creatinine level ≥ 1.5 mg/dL.
The mean difference between baseline and peak creatinine values was significantly greater in patients with AKI compared with non-AKI patients (table 1).
A Worthwhile Risk
“As we move toward a model of acute thrombectomy on more and more patients, we know that faster intervention is better,” shared Wade S. Smith, MD, PhD of the University of California, San Francisco (San Francisco, CA) in an email correspondence with WLNCMD. “It is clear that CT angiography helps more effectively triage patients and also select patients who will best benefit from neurointervention. Toward that end, one needs to administer contrast at least twice: during the initial diagnostic CTA (and perfusion if done) and second during the neurointervention.”
Contrast nephropathy is a function of the dose of contrast combined with the duration over which the contrast is given as well as renal function at that time,” Dr. Smith explained. “One can judge renal function by measuring a serum creatinine prior to contrast administration but that takes time, upwards of 30 minutes. So, many centers now give contrast before obtaining a serum creatinine in patients with no known history of renal failure.”
Previous work by Smith’s group reported that this process is safe, and that the incidence of contrast nephropathy requiring intervention is “acceptably low” (0.2%). The current paper supports that view, he added.
Dr. Smith explained that serum creatinine values available following CT imaging can be used to determine the feasibility of proceeding to thrombectomy and the need for renal protective strategies. But even if reversible kidney injury does occur, often the ultimate benefits of thrombectomy outweigh the risks. Delaying CT scanning with contrast until creatinine values are available will, by modest estimate, delay thrombectomy by 20 to 30 min. “This increases the patients’ disability by nearly a month simply because of the concern over causing acute kidney injury,” he noted.
“One needs prospective data to truly measure these differences,” concluded Dr. Smith, “but given the results of this paper and prior research, the harm associated with contrast administration is minor compared to the benefits afforded by faster time to treatment.”
In the future, he said, an increasing number of patients will be moved from the prehospital setting directly to angiography, where administration of contrast is reduced to that used for the conventional angiogram alone, further diminishing the risk of nephropathy.
Source:
Hall SL, Munich S1, Cress MC, et al. Risk of acute kidney injury associated with neuroimaging obtained during triage and treatment of patients with acute ischemic stroke symptoms. J Neurointerv Surg. 2016;Epub ahead of print.
Disclosures:
- Dr. Smith receives funding from Stryker Neurovascular
- Dr. Siddiqui has financial interests in and/or serves a consulting role at Hotspur, Intratech Medical, StimSox, Valor Medical, Blockade Medical, Lazarus Effect, Codman & Shurtleff, Concentric Medical, ev3/Covidien Vascular Therapies, GuidePoint Global Consulting, Penumbra, Stryker, Pulsar Vascular, MicroVention, Blockade Medical, Covidien Neurovascular, Abbott Vascular, Snyder, Boston Scientific, Cordis, EndoTex, Medtronic, Toshiba, Micrus, Zimmer, Access Closure, Niagara Gore Medical, EPI, Primus, Guidant: research, and Kerberos.