Key Points:
- Study compares time patients with large vessel occlusion transported to endovascular-capable center vs regional hospital
- Time to revascularization significantly longer for patients brought to regional center
Transporting patients with large vessel occlusions to the closest regional hospital rather than directly to an endovascular-capable center substantially delays revascularization, according to new registry data. The findings, presented on July 27, 2016, at the Society of NeuroInterventional Surgery (SNIS) 13th Annual Meeting in Boston, MA, suggest a need for system-wide changes in how large vessel strokes are managed.
“The time delay associated with interhospital transfer is entirely due to the time between imaging at the outside hospital and departure from the outside hospital,” Michael Froehler, MD, of Vanderbilt University Medical Center (Nashville, TN), told Neurovascular Exchange. “The time during which the original treatment team is making diagnostic considerations, treatment decisions, and transfer arrangements, that’s where all the time gets lost. That’s an area to target for improvement in the systems of care.”
Using the prospect, multicenter STRATIS registry, Dr. Froehler and colleagues analyzed the timeliness of care for large vessel occlusions treated with the Solitaire Stentriever (Medtronic) within 8 hours of onset. Specifically, the investigators looked at real-world time metrics of care delivery, specific causes of delays to treatment, and time lost due to interhospital transfer.
Within the cohort of 688 patients, 157 underwent mechanical thrombectomy alone and 421 received IV tPA plus mechanical thrombectomy. Within each group, some were sent directly to an endovascular-capable center and others transferred.
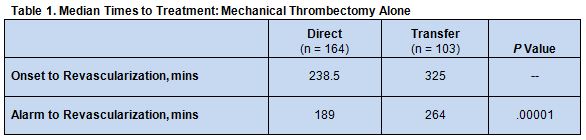
Among the thrombectomy-alone patients, median time from stroke onset to revascularization was longer with transfer versus direct transport. There was also a 75-minute time difference between these 2 groups groups with respect to alarm-to-revascularization times (table 1).
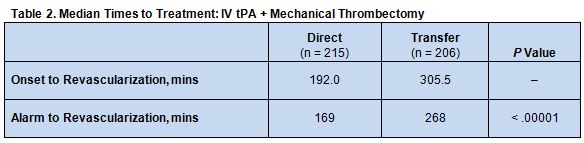
A similar pattern was seen among patients who underwent both mechanical thrombectomy plus IV tPA. In this case, patients who were transferred waited an average of 99 minutes longer from alarm to revascularization than did those who went directly to an endovascular capable center (table 2).
In both subgroups of patients, the time differences were mainly accounted for by imaging-to-transfer time at the regional hospital, which was 93 minutes for mechanical thrombectomy alone and 87 minutes for IV tPA plus mechanical thrombectomy.
Median door-to-tPA times were 56.5 minutes at regional hospitals and 38.0 minutes at the enrolling sites (P < .0001). The transfer time from a regional hospital to an endovascular-capable center was 32 minutes, for a total hypothetical time from bypass to tPA of 70 min.
Bypass-Selected Patients
According to Dr. Froehler, an important question is, “How often do we need to go to the regional hospital vs just bypassing it and going directly to the endovascular capable center?
“We looked at that in our study in two different ways,” he explained. “One was with a hypothetical bypass scenario that was created by using a very conservative measure of how long a bypass might take, which assumes the maximum distance between the scene and the endovascular capable center.” Even at a maximum distance, IV tPA would only be delayed by about 13 minutes when transporting patients directly to the endovascular capable center. This compares with a time savings of 99 minutes for access to mechanical thrombectomy.
Next, Dr. Froehler and his team will perform a route mapping analysis for each patient to help determine how bypassing regional hospitals would have affected individual patient care, he reported.
Donald Chen, MD, of Rush University Medical Center (Chicago, IL), explained that the current system of taking suspected stroke patients to the nearest hospital was set up when their treatment was quite different.
“Stroke care was designed around developing numerous primary stroke centers that could deliver IV tPA [within a certain time frame],” he said. “But patients identified with large vessel occlusions, who are better suited for treatment with thrombectomy vs IV tPA, still get caught up in the whole workup for IV tPA rather than being more quickly transported to places that can provide endovascular therapy.
“Meanwhile, the brain is holding its breath, [which] decreases the chance of a good outcome,” Dr. Chen stressed.
Now that mechanical thrombectomy has been shown to be a superior treatment option for many large vessel occlusions, said Donald Frei, MD, of Radiology Imaging Associates (Denver, CO), a major focus in neurointerventional care is to train paramedics and emergency medical services (EMS) staff to recognize large vessel occlusions in the field and transport these patients directly to an endovascular capable hospital. Dr. Frei, who is immediate past president of the SNIS, added that studies such as this one are helping to drive important changes in systems of care.
There are several quick and easy-to-use scales with a high sensitivity for detecting large vessel occlusions that EMS staff could use in the field, said Dr. Frei. These include the Rapid Arterial oCclusion Evaluation (RACE) and the Cincinnati Prehospital Stroke Severity Scale (CPSSS). In addition, the SNIS is developing an app specifically designed for this purpose, he noted.
Source:
- Froehler M, Aziz-Sultan M, Jahan R, et al. Systems of care efficiency and interhospital transfer delays in the STRATIS registry. Presented at: SNIS 13th Annual Meeting. July 27, 2016. Boston, MA.
Disclosures:
- Dr. Froehler reports being a consultant for Medtronic Neurovascular and a steering committee member for the STRATIS registry.
- Drs. Chen and Frei report no relevant conflicts of interest.