Key Points:
- Study looks at effectiveness of single operator’s effort to adopt techniques for reducing radiation exposure
- Radiation exposure reduced in both adult, pediatric patients
It is indeed feasible to reduce radiation exposure during diagnostic cerebral angiography without sacrificing diagnostic accuracy, at least according to one operator’s experience in adopting new techniques. The findings were published online April 7, 2016, ahead of print in the Journal of NeuroInterventional Surgery.
Monica S. Pearl, MD, of Johns Hopkins University School of Medicine (Baltimore, MD), and colleagues reviewed the first 50 consecutive adult and pediatric patients in whom she performed diagnostic cerebral angiography each year from 2010 to 2013. For each patient, radiation exposure based on angiogram and procedure examination protocols were analyzed according to patient age, gender, diagnosis, angiography techniques, and fluoroscopy time.
Data were reviewed for 200 adults and 31 children. Adult patients were aged from 19 to 94 years. Pediatric patients were aged from 2 to 18 years. Approximately 6 in 10 were women.
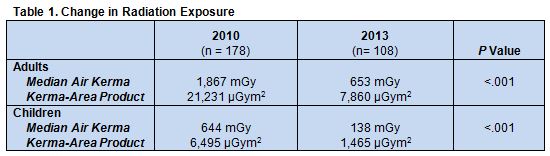
From 2010 to 2013, median air kerma and kerma-area product decreased in both adults and children, during which time Dr. Pearl adopted several practical techniques for minimizing radiation exposure that she has outlined in a previous publication. They involved modifying DSA frame rate, fluoroscopic and roadmap pulse rates, and flat panel detector position (table 1).
“In our field, there is growing concern about exposure during neurointerventional procedures, but it may not be a priority for some people,” Dr. Pearl told WLNCMD in a telephone interview. The goal of this paper, she said, was two-fold: to increase awareness about the importance of decreasing radiation exposure for both patients and operators and to demonstrate that it is feasible to do so without compromising diagnostic accuracy.
“Neurointerventional techniques have revolutionized diagnosis and management, but they come at a price,” said Dr. Pearl. Operators must keep in mind that patients often undergo multiple procedures and imaging that can result in high cumulative radiation exposure. “Every opportunity you have to reduce exposure while maintaining diagnostic accuracy should be used.”
“It’s basically about changing your habits,” she explained. “You need to know to your equipment, . . . not just how to operate it, but what the radiation dose is per frame or per pulse on each setting. If you’re not familiar with it, arrange to have an applications training session with the vendor.”
At the end of each procedure, she recommended, operators should analyze their exam protocol, including the number of runs, radiation dose per run, and fluoroscopy time and dose. Analyzing one’s own trends makes it possible to modify machine settings and techniques. “It has to be a priority for the operator, to recognize it is important and take responsibility to do it not only for the patient, but for themselves and everyone else in room,” she said. That means getting away from the habit of producing “picture perfect” images and focusing instead on individualizing each exam to produce images that are just clear enough to be diagnostic.
Concerns about radiation dose during neurointerventional testing took hold following a 2010 New York Times article that highlighted cases of accidental overexposure to radiation among patients receiving CT brain perfusion in California, Joseph J. Gemmete, MD, of the University of Michigan Health Centers (Ann Arbor, MI), told WLNCMD in a telephone interview. Since then, professional organizations such as the American College of Radiology have made a concerted effort to educate their members about the importance of paying attention to radiation exposure, both for patients and physicians.
“We are concerned about radiation,” he said, “but a lot times we ignore the outward side effects that radiation causes because it is delayed. You don’t see them up front, so the cause and effect is not [immediately obvious].”
In addition to adopting the methods outlined by Dr. Pearl—which Dr. Gemmete said are techniques familiar to most operators even if they are not universally adopted—he suggested that imaging technology vendors should be encouraged to adapt their equipment, so that better images can be produced with less radiation exposure. Philips Healthcare already offers dose reduction schemes, he noted.
Source:
- Schneider T, Wyse E, Pearl MS, et al. Analysis of radiation doses incurred during diagnostic cerebral angiography after the implementation of dose reduction strategies. J NeuroInterv Surg. 2016;Epub ahead of print.
Disclosures:
- Drs. Pearl and Gemmete report no relevant conflicts of interest.