Key Points:
- Study compares outcomes of endovascular stroke therapy with and without IV-tPA
- Rates of reperfusion, good outcome similar for both groups if treated early
Patients with acute ischemic stroke due to large vessel occlusions can benefit from endovascular therapy even if they are not eligible to intravenous tissue plasminogen activator (IV tPA), provided they can be treated early enough. These are the main findings of a retrospective analysis published in the April 2016 issue of Stroke.
Raul G Nogueira, MD, of Grady Memorial Hospital (Atlanta, GA), and colleagues retrospectively analyzed a prospectively collected database of 422 consecutive patients who were treated with endovascular therapy within 6 hours of stroke onset between September 2010 and April 2015. Outcomes were compared between the 253 (59%) patients treated with IV tPA prior to endovascular therapy and the 169 (41%) who did not receive IV tPA because of ineligibility.
Overall, patients who received IV tPA were slightly younger (mean 64.9 vs. 67.9 years, P = .05), more often male (56% vs. 44%, P = .01), and less likely to have hypertension (70% vs. 81%, P = .02) and vertebrobasilar occlusions (3% vs. 8%. P = .02) than those who did not. The 2 groups were similar with respect to National Institutes of Health Stroke Scale (NIHSS) score, Alberta Stroke Program Early CT Score (ASPECTS), and stroke onset to puncture times.
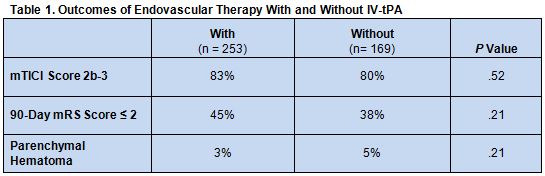
Following endovascular therapy, there were no differences between the two patient groups with respect to the rates of successful reperfusion (mTICI 2b-3), good outcome (mRS score ≤ 2) at 90 days, or any parenchymal hematoma (table 1).
While unadjusted 90-day mortality was higher among those who did not receive IV tPA (21% vs. 34%, P < .01), logistic regression analysis revealed that IV-tPA ineligibility was not associated with differences in mTICI 2b-3, parenchymal hematoma, or 90-day good outcome or mortality.
“Our findings suggest that patients who are ineligible for IV tPA who presented [for endovascular therapy] within 6 hours of symptom onset can safely undergo [the treatment] and seem to achieve similar rates of reperfusion and good outcome compared with [patients who do receive IV tPA and undergo endovascular therapy] within the same time frame,” write the authors.
IV tPA Ineligibility ‘Not Uncommon’
“It is not uncommon in clinical practice to come across patients presenting with acute ischemic stroke due to large vessel occlusion who have one or more contraindications to IV tPA, including delayed presentation, coagulopathy, recent stroke, gastrointestinal hemorrhage or surgery, and suspected septic embolism,” Perry Ng, MD, of the University of Utah Health Sciences Center (Salt Lake City, UT), told WLNCMD in an email.
“IV tPA has been routinely used in eligible patients with acute ischemic stroke but is less effective in large vessel occlusion”, he noted. “Several recent randomized controlled trials showed a benefit of endovascular therapy after IV tPA in large vessel occlusions using stent retrievers, especially when recanalization can be achieved early.”
The current findings, Ng said, indicate that IV tPA-ineligible patients can also benefit from an endovascular approach. “What they do not mean,” he emphasized, “is that patients who are eligible for IV tPA should have endovascular therapy in lieu of IV tPA or have IV tPA withheld while awaiting or considering endovascular therapy.”
Source:
- Rebello LC, Haussen DC, Grossberg JA, et al. Early endovascular treatment in intravenous tissue plasminogen activator-ineligible patients. Stroke. 2016;47:1131-1134..
Disclosures:
- Dr. Nogueira reports receiving support from Stryker Neurovascular, Covidien, and Penumbra.
- Dr. Ng reports no relevant conflicts of interest.