Key Points:
- One in 12 patients develop restenosis within 2 years after CAS
- CAD, history of cerebrovascular accident, greater stenosis at baseline increase risk
Investigators led by Stavropoula Tjoumakaris, MD, of Thomas Jefferson University Hospital (Philadelphia, PA), retrospectively analyzed 241 patients (mean age 67.5 years; 57.3% men) treated with CAS for symptomatic and asymptomatic carotid artery stenosis between February 2003 and November 2011.
Overall, 8.3% of the patients developed carotid restenosis of ≥ 50% and 3.7% required retreatment during a median follow-up period of 24 months. Mean duration from stenting to retreatment was 11 months.
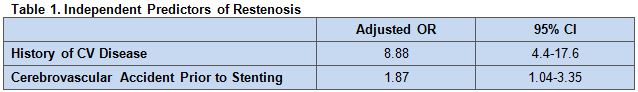
On multivariate analysis, independent predictors of restenosis included history of cardiovascular disease and having a cerebrovascular accident prior to stenting (table 1).
In addition, univariate analysis revealed an increasing odds of restenosis with greater preoperative carotid stenosis (P = .04) with an almost six-fold increased risk for stenosis ≥ 80%.
There were trends toward increased restenosis in patients who had received prior CAS or endarterectomy and greater need for retreatment in patients with a higher degree of pretreatment stenosis.
Risk Factors Could Inform Patient Selection
“Patients with a higher degree of carotid stenosis may be at a higher risk of having residual disease that can act as a focus for myointimal hyperplasia,” Dr. Tjoumakaris and colleagues write. “Furthermore, these patients may be at a higher risk of progression of atherosclerotic disease leading to carotid restenosis.”
The findings suggest that while the rate of carotid restenosis is low after CAS, certain risk factors should be paid close attention in order to avoid complication. The choice between endarterectomy and CAS “should be carefully considered” in patients with a history of cardiovascular disease or cerebrovascular accident, the study authors write, adding that “the long-term risk of restenosis should be kept in mind when opting for stenting in these patients.”
Study Lacks Ultrasound Data
Among the limitations of the study are the small number of patients who developed restenosis, its single-center design, and its retrospective nature, the study authors say. The latter factor means that “follow-up periods were not constant for all patients,” they note. “However, most of the outcomes of interest occurred early within the first 2 years after CAS.”
But Dr. Christopher White, MD, of the Ochsner Heart and Vascular Institute (New Orleans, LA), noted other limitations in an email to WLNCMD. In addition the study’s small sample size, he said, it fails to mention the ultrasound criteria for restenosis. In research published in 2007, Dr. White and colleagues demonstrated how peak systolic velocity (PSV) and internal carotid artery to common carotid velocity ratio (ICA/CCA), as measured by ultrasound, can be used to identify in-stent restenosis. They determined that a peak of 240 cm/sec and an ICA/CCA ratio of 2.45 are optimal thresholds to diagnose > 50% in-stent restenosis, and a PSV of 450 cm/sec and ICA/CCA ratio of 4.3 are optimal thresholds to diagnose > 70% in-stent restenosis.
Source:
Daou B, Chalouhi N, Starke RM, et al. Predictors of restenosis after carotid artery stenting in 241 cases. J NeuroIntervent Surg. 2015;Epub ahead of print.
Disclosures:
- Drs. Tjoumakaris and White report no relevant conflicts of interest.