But the strategy failed to reduce the incidence of delayed cerebral ischemia, which was the study’s primary endpoint.
Use of high-dose heparin does not reduce the rate of delayed cerebral ischemia (DCI) among patients who undergo endovascular treatment of aneurysmal subarachnoid hemorrhage, according to a retrospective analysis published online last month in Neurosurgery. However, the authors identified enough other potential clinical benefits that they felt justified calling for a randomized, prospective trial of the therapy.
DCI occurs in as many as 40% of patients with aneurysmal subarachnoid hemorrhage and “significantly contributes to poor outcome and death,” write investigators led by Rene Post, MD (Academic Medical Center Amsterdam, the Netherlands). They point out that treatment approaches for DCI vary widely. While there is some evidence that heparin may play a role in preventing the complication, clinical data remain unclear.
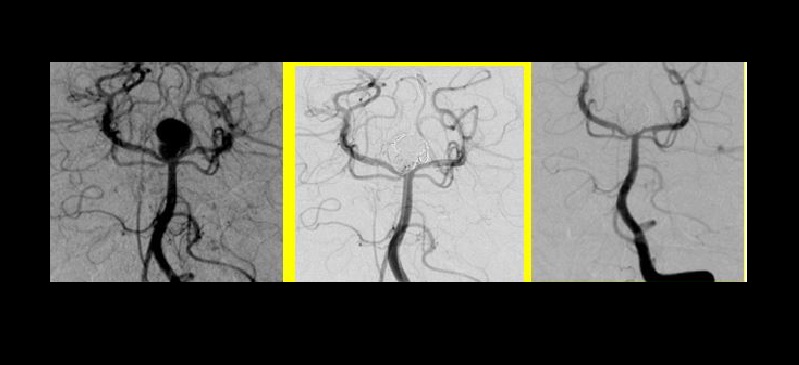
Over their 2-year study, Post and colleagues treated patients with high-dose nadroparin from after endovascular therapy until discharge. “The aim of this study was to assess whether these patients developed less DCI than patients who, in the period thereafter, were treated with low-dose nadroparin,” they explain. “Our secondary aim was to assess whether outcome was better in these patients."
The investigators analyzed the medical records of 158 adult patients who underwent clipping for aneurysmal subarachnoid hemorrhage: 93 received high-dose nadroparin (twice daily subcutaneous injections of 5,700 AxaIU) and 65 received low-dose nadroparin (once daily subcutaneous injections of 2,850 AxaIU). Patients’ medical charts were reviewed and imaging was scored by two independent neuroradiologists.
There were no significant differences between the two groups of patients with respect to the occurrence of clinical DCI. However, after adjusting for neurological status on admission, a larger proportion of patients given the high-dose treatment were discharged to home. In-hospital mortality was also lower in the high-dose group, even after again making similar adjustments.
High- vs Low-Dose Nadroparin
|
|
OR (95% CI) |
|
Clinical DCI |
1.18 (0.60-2.33) |
|
Discharge to Home (Adjusted) |
3.13 (1.36-7.24) |
|
In-Hospital Mortality |
0.19 (0.07-0.55) |
|
Mortality (Adjusted) |
0.21 (0.07-0.63) |
Confirmatory Trial Needed
The authors point out that their study differs from other published studies on use of heparin to prevent DCI in that it exclusively involved patients treated endovascularly and employed heparin in a dose high enough to have an anticoagulation effect.
“Our data suggest that treatment with high-dose subcutaneously administered low-molecular-weight nadroparin is safe, and leads to more favorable clinical outcome, favoring discharge to home, although it did not reduce [clinical] DCI in our patient cohort,” they write. They recommend that a prospective randomized controlled trial be conducted to confirm the benefits of this intervention.
Maxim Mokin, MD, PhD (University of South Florida, Tampa, FL), in a commentary accompanying the study, points out an important limitation: the manner in which DCI was measured.
“Gathering data on the occurrence of clinical DCI in a retrospective study could result in a substantial error,” he writes. “Similar limitations apply to the radiographic assessment of infarcts on follow-up imaging without the use of standardized imaging protocols.”
Despite these limitations, Mokin does acknowledge that the study still indicates that high-dose heparins may be beneficial in this context and that prospective trials are warranted.
Source:
Post R, Zijlstra IAJ, van den Berg R, et al. High-dose nadroparin following endovascular aneurysm treatment benefits outcome after aneurysmal subarachnoid hemorrhage. Neurosurgery. 2017;Epub ahead of print.
Disclosures:
Post and Mokin report no relevant conflicts of interest.

