Key Points:
- Multicenter study reviews outcomes of thrombectomy for posterior strokes
- Half of patients have good outcomes if identified, treated within 6 hours of stroke onset
Patients with posterior circulation strokes have a high likelihood of good outcome with prompt thrombectomy, according to research presented on February 17, 2016, in Los Angeles, CA, at the 2016 International Stroke Conference.
The findings also were published online ahead of print in Stroke.
“Recent randomized stroke trials (MR CLEAN, ESCAPE, SWIFT PRIME, EXTEND-1A, and REVASCAT) excluded patients with posterior circulation strokes, and only a small percentage of patients with posterior circulation strokes were included in SYNTHESIS (10%) and IMS III (2%),” Maxim Mokin, MD, PhD, of the University of South Florida (Tampa, FL), told WLNCMD in an email. In earlier trials, he added, “currently available thrombectomy approaches (stent retrievers and distal aspiration catheters) were not used.”
To home in on posterior stroke, Dr. Mokin and colleagues performed a multicenter retrospective analysis of 100 consecutive patients (mean age 63.5 years; 33% women) who underwent thrombectomy with stent retrievers or primary aspiration thrombectomy (including A Direct Aspiration First Pass Technique [ADAPT] approach) for posterior circulation strokes. Patients’ mean National Institutes of Health Stroke Scale (NIHSS) score was 19.2.
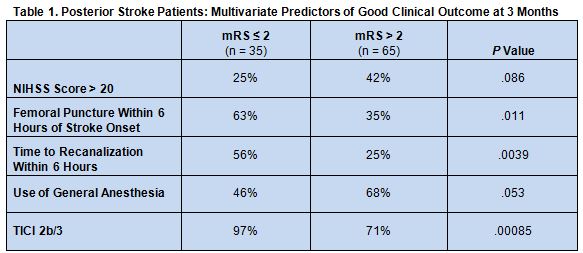
At 3 months, 35% of patients achieved a favorable clinical outcome, defined as a modified Rankin Scale (mRS) score ≤ 2. Significant predictors of good outcome on multivariate analysis were successful recanalization and shorter time from stroke onset to procedure start. There was also a trend toward decreased likelihood of good outcomes among patients with an NIHSS score > 20 and with use of general anesthesia (table 1).
Use of a stent retriever or aspiration thrombectomy as the primary treatment approach did not significantly affect clinical outcome. None of the baseline advanced imaging modalities (MRI, CT perfusion, or CT angiography assessment of collaterals) showed superiority in selecting patients for thrombectomy.
Early Intervention Key
“We were amazed to see that early treatment leads to [half having] good clinical outcomes at 3 months,” noted Dr. Mokin. “Given the poor natural history of posterior circulation strokes, such a number is remarkable. We [achieved that outcome] despite differences in imaging protocols and types of treatment.”
According to Dr. Mokin, “some institutions treat posterior circulation strokes with endovascular therapies up to 24 hours from stroke symptoms onset, sometimes administering IV thrombolysis first and waiting for clinical improvement before committing to thrombectomy.”
This type of stroke also “can be difficult to recognize clinically, leading to delay to treatment,” Dr. Mokin noted. Based on the current findings, he advised, “practices need to change to ensure that patients with posterior circulation strokes due to large vessel occlusion are taken for thrombectomy immediately.”
Dr. Mokin also pointed out that available research into selection criteria for thrombectomy applies primarily to anterior circulation strokes. There remains a need to “expand our knowledge on the role of ASPECTS, CT perfusion, and MRI selection criteria for posterior circulation strokes,” he noted. “Also, the updated 2015 AHA guidelines do not provide significant guidance on this population of patients, creating confusion among the ER and stroke neurology community. We need to address this issue as well.”
Source:
Mokin M, Sonig A, Sivakanthan S, et al. Clinical and procedural predictors of outcomes from the endovascular treatment of posterior circulation strokes. Stroke. 2016;Epub ahead of print.
Disclosure:
- Dr. Mokin reports no relevant conflicts of interest.