The new guidelines emphasize the importance of having an appropriate care team and dealing with complications.
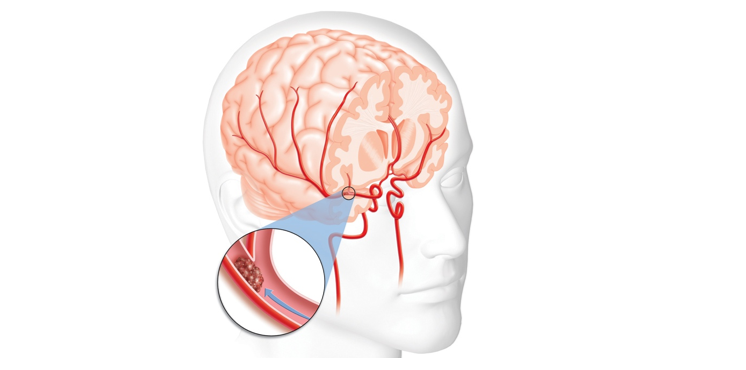
The Society for NeuroInterventional Surgery (SNIS) has developed guidelines specifically targeted at the management of patients who undergo mechanical thrombectomy for emergent large vessel occlusions (ELVOs).
Lead author and chair of the SNIS Standards and Guidelines Committee Justin Fraser, MD (University of Kentucky, Lexington, KY), told Neurovascular Exchange that this particular document belongs to a set of past and upcoming guidelines that address how to manage patients who have received mechanical thrombectomy, currently a hot topic in stroke care. While other guidelines focus on issues such as triage, recognition, training, and technical aspects of the procedure, this series takes aim at postprocedural care.
He emphasized that at the SNIS has no intention of policing its members. Rather, “we view our role as providing a foundation for the practice of neurointerventional radiology,” Fraser said. “Our job is to critically evaluate the literature, pose and answer questions about practice, and assimilate the literature into standards of practice.”
The guidelines were published online September 29, 2017, ahead of print in the Journal of NeuroInterventional Surgery.
Guideline Summary
The guidelines are divided into main topics, each containing a brief review of the literature, key recommendations, and their levels of evidence:
1. Postthrombectomy care environment
a. Inpatient care in a designated stroke unit with access to a coordinated multidisciplinary team is required to optimize the potential for functional independence.
b. Comprehensive stroke centers or the local equivalent are most likely to provide postprocedural care that is specific to patients’ needs. Stroke units should therefore be prioritized for ELVO patients after thrombectomy.
2. Preserving threatened tissue (failed or incomplete recanalization)/therapeutic hypertension
a. In patients with unsuccessful or partially successful recanalization, consider sustaining ischemic penumbral tissue through hemodynamic support through induced hypertension and patient positioning. Collateral support should continue for at least 24 hours before attempts to wean.
3. Complication avoidance and management
a. Employ postoperative imaging to monitor for postthrombectomy hemorrhage.
b. After reperfusion, blood pressure management should take into account baseline blood pressure ranges, balancing reperfusion needs against the risk of hemorrhage.
c. Consider reversal of tPA in patients experiencing significant bleeding complications from tPA.
4. Malignant cerebral edema
a. Utilize clinical and imaging data to identify patients at high risk for malignant cerebral or cerebellar edema.
b. Employ regular, frequent neurological examinations to follow level of arousal, pupillary findings, and motor responses in at-risk patients.
c. Early imaging findings that demonstrate significant tissue involvement within the first 6 hours predict significant cerebral edema.
d. Steps can be taken to manage and monitor cerebral edema when it occurs.
5. Access-site complications
a. Closure devices are useful in the appropriate clinical context, with similar complication rates. There is a modest advantage of immediate hemostasis that may allow for faster patient mobilization postprocedure.
b. Significant complications can develop acutely or subacutely at the access site, so investigations and interventions may be urgently or emergently needed. Appropriate and standardized monitoring is needed.
6. Postprocedural rehabilitation
a. All patients should have an initial assessment by multidisciplinary rehabilitation professionals as soon as possible after admission.
b. Due to rehab’s impact on outcome, make every effort to place patients in a program.
c. Ninety-day outcome assessment after thrombectomy is a reasonable and appropriate standard follow-up.
According to Steven Giannotta, MD (University of Southern California, Los Angeles, CA), some of the most important and relevant features of these guidelines relate to the care environment. Many hospitals are under the impression that becoming a stroke center is as simple as hiring an interventionalist, but good stroke care requires much more, he said.
“Not only do you need personnel with expertise, but you need a care system,” he explained to Neurovascular Exchange. Enough resources and staffing must be made available to achieve not only neurointerventional and neurosurgical services, Giannotta said, but also neurocritical care services 24/7.
“No matter what a neurointerventionalist does in terms of pulling a blood clot out of a blood vessel, the patient is going to croak in your ICU if there are no available doctors on call over the weekend or there are no neurocritical care people physically in the hospital [with] all of the appropriate neurocritical care resources,” Giannotta emphasized. This is particularly true, he said, for patients who develop cerebral edema.
Fraser also highlighted the need for a coordinated approach. “Having a specific team of people who are trained to take care of stroke patients in specific locations . . . that can bring the same standard of care to every patient is important,” he said, encouraging neurointerventionalists to take an active role not just in procedures but also in pre- and poststroke care.
Another key feature of the guidelines, Fraser observed, is the need to look for and minimize cerebral edema as well as the role of decompressive craniectomy. He pointed out brain swelling can and does happen following thrombectomy, stressing that neurointerventionalists need to know how to treat it.
Finally, Giannotta noted that the guidelines appropriately distinguish between typical outcomes for younger versus older patients. “After 60, the population-based results are never going to be as good and response to mitigation of complications is less,” he said. “Patients over 60 are much less likely to become functional, so it is important to manage expectations.”
Source:
Leslie-Mazwi T, Chen M, Yi J, et al. Post-thrombectomy management of the ELVO patient: guidelines from the Society of NeuroInterventional Surgery. J NeurInterv Surg. 2017;Epub ahead of print.
Disclosures:
- Fraser reports involvement with Fawkes Biotechnology and Stream Biomedical, both of which are involved in development of neuroprotective tools and devices.
- Giannotta reports no relevant conflicts of interest.

