Key Points:
- Single-center study examines complications, outcomes of intracranial stenting over 1 year
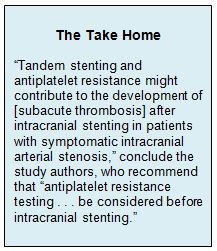
- Tandem stenting, antiplatelet resistance both risk factors for subacute thrombosis
Zhongrong Miao, MD, of Beijing Tiantan Hospital (Beijing, China), and colleagues prospectively collected data on all 221 patients treated for symptomatic intracranial arterial stenosis using intracranial stenting in 2013 at their hospital. Among these patients, 9 (4.1%) developed subacute thrombosis 2 to 8 days following stenting.
They note that the 4.1% rate of subacute thrombosis identified in this series was lower than that previously reported by Riedel et al but higher than that reported in the SAMMPRIS trial.
Binary logistic analysis revealed that tandem stenting and antiplatelet resistance were both predictors of the development of subacute thrombosis (table 1).
Table 1. Factors Associated With Increased Odds of Subacute Thrombosis
|
|
Odds Ratio (95% CI) |
|
Tandem Stenting |
11.28 (2.42-52.52) |
|
Aspirin Resistance |
6.27 (1.57-24.95) |
|
Clopidogrel Resistance |
15.53 (3.11-77.63) |
|
Aspirin and Clopidogrel Resistance |
12.25 (2.93-51.15) |
|
Aspirin or Clopidogrel Resistance |
11.34 (2.28-56.34) |
Testing for Antiplatelet Resistance Important
Stent thrombosis is “one of the devastating complications that may occur after stent placement,” the study authors say. Despite its clinical importance, this study is among the few that have evaluated potential risk factors for its occurrence in intracranial stenting.
They conclude from their findings that “antiplatelet resistance testing should be considered before intracranial stenting,” reporting that in their center they have begun a strategy of increasing the dose of aspirin or clopidogrel among patients with evidence of inadequate inhibition. They also suggest that cilostazol could be another option, as are heparin-coated stents. At present, there is “no consensus on the best treatment regimen to overcome this problem,” the authors write, recommending that the relative benefits of each strategy undergo further investigation.
Source:
Sun X, Tong X, Lo WT, et al. Risk factors of subacute thrombosis after intracranial stenting for symptomatic intracranial arterial stenosis. Stroke. 2017;Epub ahead of print.
Disclosures:
Dr. Miao reports no relevant conflicts of interest.

