- Key Points:
- - Two studies look at potential utility of clot burden score in mechanical thrombectomy for acute ischemic stroke
- - One reveals good results across all scores, the other shows better outcomes with higher clot burden
Two new studies, one published online September 15, 2016, in the Journal of NeuroInterventional Surgery and the other online November 8, 2016, in Stroke, use data from recent pivotal trials to help determine what this quick and easy-to-calculate marker really means clinically.
SWIFT PRIME Data
For the JNIS paper, Maxim Mokin, MD, of University of South Florida Neurosurgery (Tampa, FL), and colleagues divided the 69 patients who were part of the endovascular arm of SWIFT PRIME into 3 groups based on their CBS: 0-5 (n = 14), 6-7 (n = 23), and 8-9 (n = 32). They found no difference in clinical characteristics among the groups, with the exception of baseline Alberta Stroke Program Early CT Score (P = .049) and site of proximal occlusion (P < .001).
Rates of successful recanalization (defined as TICI 2b/3), complete recanalization (defined as TICI 3), and good clinical outcome at 3 months (defined as mRS 0-2), were similar among the three groups.
MR CLEAN Data
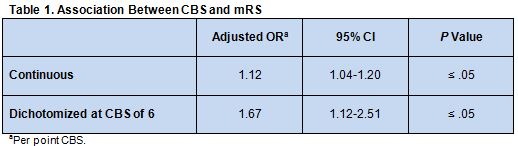
In the second study, Kilian M. Treurniet, MD, of the Academic Medical Center (Amsterdam, the Netherlands), and colleagues calculated CBS for 499 of the 500 MR CLEAN patients. They used ordinal logistic regression models with and without including main baseline prognostic variables to determine its relationship with mRS.
They found that a higher CBS was associated with a shift toward a better mRS (table 1). Both effect estimates were slightly attenuated by adding baseline prognostic variables, but adding interaction terms did not significantly improve the fit of the models.
There was a small and insignificant increase of intra-arterial treatment efficacy in the high CBS group.
In an email to Neurovascular Exchange, Dr. Mokin indicated that he is not surprised that the two studies yielded somewhat different findings, given the differences in patient populations. “Our study used very strict imaging inclusion criteria, whereas the study based on the MR CLEAN data set was a more pragmatic study with wider inclusion criteria,” he pointed out. “Also, our study only included patients treated with a specific type of stent retriever (Solitaire), [whereas the other] was based on a population treated with various devices and approaches to thrombectomy.”
Dr. Treurniet, also via email, told NeuroVascular Exchange that rates of successful reperfusion were higher in SWIFT PRIME than MR CLEAN, which could also contribute to the different outcomes. In the SWIFT PRIME-based study, a nonsignificant trend was seen toward better mRS scores with a higher CBS, he added.
Tweaking the Approach to Improve Outcomes
Together, “these two studies tell us that different types of occlusion, depending on how large or small the clot burden is, respond differently to mechanical thrombectomy therapies that we currently rely on in our practice,” said Dr. Mokin.
Proper interpretation of the findings is critical, he emphasized. “Evidence for efficacy of thrombectomy in stroke is strong, and we should NOT base our decision on whether to intervene on the clot burden score or other factors describing the nature and characteristics of the clot (eg, clot density, clot composition).
Another recent study has also shown that clot burden is not a barrier to mechanical thrombectomy in the posterior circulation. In concert, said Fatih Seker, MD, of Heidelberg University Hospital (Heidelberg, Germany), “these studies tell us that mechanical thrombectomy using stent-retrievers is effective in removing intracranial thrombi, no matter if short or long.”
“One can doubt the necessity of analyzing thrombus extent,” he wrote in an email, citing his own research showing “that thrombus length does not correlate with thrombectomy maneuver count needed for recanalization. Finally, high clot burden is no contraindication for thrombectomy.”
But CBS can still be useful in that it is quick and easy to calculate in all patients, Dr. Mokin said. “Now that we have access to various thrombectomy approaches and devices, . . . we are starting to gather data on which device is better for which type of clot.”
Dr. Treurinet warned against using a single variable—such as poor collaterals—to guide treatment selection, but he agreed that CBS could have an important role to play in guiding therapy. “It might be of interest in the near future when decisions need to be made concerning rt-PA treatment before mechanical thrombectomy,” he said. “We know the effect of rt-PA is limited in patients with a bigger clot burden, so patients with a low clot burden score (ie, high clot burden) might not need additional rt-PA administration.”
It would be interesting, Dr. Treurinet said, to further investigate whether reperfusion rates can be improved “by developing new treatment strategies for patients with a big clot burden. Further, thrombus characteristics in general currently are a hot topic of research. Thrombus permeability, clot burden, and length of the clot might play a big role in the upcoming question whether or not to administer rt-PA before mechanical thrombectomy.”
Dr. Mokin looks to a future in which interventionalists “decide which particular device [to use] based on evidence of how it performs in cases specific to clot burden score and other imaging markers.”
Results of ongoing studies in which endovascular therapy is “tweaked” to specifically address very large or small clots are anticipated.
Sources:
- Mokin M, Levy EI, Siddiqui AH, et al. Association of clot burden score with radiographic and clinical outcomes following Solitaire stent retriever thrombectomy: analysis of the SWIFT PRIME trial. J NeuroInterv Surg. 2016;Epub ahead of print.
- Treurniet KM, Yoo AJ, Berkhemer OA, et al. Clot burden score on baseline computerized tomographic angiography and intra-arterial treatment effect in acute ischemic stroke. Stroke. 2016;Epub ahead of print.
Disclosures:
Drs. Mokin, Treurniet, and Seker report no relevant conflicts of interest.