Key Points:
- Registry study compares mechanical thrombectomy for M1 versus M2 stroke lesions
- Mortality, intracranial hemorrhage, and 90-day function similar for patients in both groups after treatment
Registry data on patients experiencing acute stroke are demonstrating that mechanical thrombectomy is as safe, feasible, and effective for M2 lesions as it is for M1 occlusions. The findings were presented on July 25, 2016, at the Society of NeuroInterventional Surgery (SNIS) 13th annual meeting in Boston, MA.
“Most prospective, clinical, randomized thrombectomy trials have a limited number of M2 occlusions, and some even excluded them,” researcher Osama Zaidat, MD, of St. Vincent Mercy Medical Center (Toledo, OH), told Neurovascular Exchange. “But in real life, the M2 is an important artery, and people go after it frequently. Registries provide a good venue to have a large sample of M2 occlusions.”
For the study, Zaidat and colleagues used data from the investigator-initiated Trevo Acute Ischemic Stroke (TRACK) registry. The dataset consisted of 631 consecutive patients with acute ischemic stroke who were treated at one of 23 clinical centers: 84 patients (13%) had M2 and 344 (54.5%) had M1 occlusions. Mean age was similar between groups, as were time of onset to groin puncture and total procedure time. However, patients with M2 lesions had lower baseline National Institutes of Health Stroke Scale (NIHSS) scores (median 14 vs 18; P = < .0001).
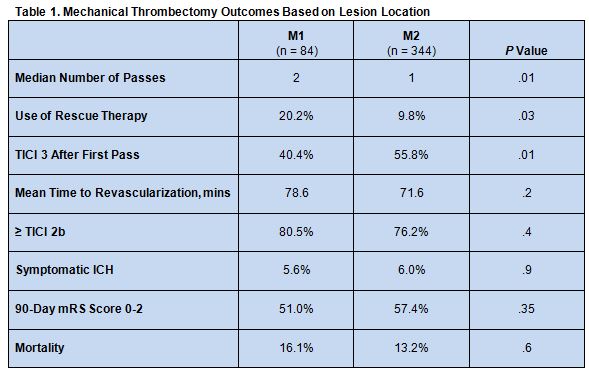
The number of passes needed to achieve recanalization with the Trevo device was higher for the M1 group than the M2 cohort, and M1 patients were also more likely to require rescue therapy. Patients with M2 occlusions also had higher rates of TICI 3 revascularization after the first pass. On the other hand, both groups were similar with respect to time to revascularization, revascularization success, and rates of symptomatic intracranial hemorrhage (ICH), 90-day mRS score 0-2, and mortality (table 1).
Dr. Zaidat expressed surprise at finding that recanalization was achieved in 1 pass more commonly in M2 than M1 occlusions but that the overall rate of recanalization was statistically similar for both arteries. “I was thinking that M2 was easier to go after, and you should be able to recanalize it more often,” he said.
He speculated that perhaps smaller clots fragment more easily and interventionalists working on M2 arteries are less concerned than perhaps they should be about leaving small clots or fragments behind.
According to Dr. Zaidat, the study “really brings home that [M2] is an important branch to treat.” When working one of these lesions, operators should not give up easily by ignoring distal fragments, he advised. “We should give it a full [opportunity] to achieve a high rate of recanalization.”
He hopes that smaller, newer-generation devices, such as the 3-mm Trevo, will allow interventionalists to integrate the clot in M2 occlusions more effectively, resulting in better outcomes. When these findings are published, said Dr. Zaidat, they will include an analysis that examines whether use of the 3-mm TREVO had an impact on outcome.
M2 Thrombectomy a Good ‘Return on Investment’
Donald Frei, MD, of Radiology Imaging Associates (Denver, CO), who is immediate past president of the SNIS, pointed out that the study is particularly enlightening in light of other results presented at the meeting. In the other study, he said, von Kummer et al showed that longer clots are more difficult to recanalize and are associated with poorer outcomes. Taken together, both studies confirm that the greater the clot burden, the more difficult it is to remove the clot and return patients to independence.
“What’s happening in parallel is we have a lot of incremental improvement in endovascular technology that can tackle even the most difficult clots,” said Dr. Frei. “The technology continues to improve, and the tools are getting better.”
According to Michael Chen, MD, of Rush University Medical Center (Chicago, IL), the TRACK registry data demonstrate that the “return on investment” for treating M2 occlusions is largely worthwhile. “The concern [for M2 vs M1 occlusions] would be that these patients may not have strokes that are that big, and you’re putting a device in a vessel that is much smaller, . . . which may have a higher risk for hemorrhage and may not pay off in terms of patient benefit. What this study shows is that, in fact, those lesions [can be treated safely],” he explained.
The lack of a control group of patients with M2 lesions who did not undergo mechanical thrombectomy means the study fails to address whether M2 occlusions are better treated with or without an endovascular approach, said Dr. Chen. But given that hemorrhage is the most concerning complication of endovascular therapy and the risk of symptomatic ICH was no higher with M2 than M1 occlusions, he concluded, it still strongly supports thrombectomy, especially for M2 occlusions that occur in eloquent parts of the brain, such as areas responsible for motor function or language.
Source:
- Castonguay A, Nogueira R, English J, et al. Analysis of M2 occlusions within TREVO Acute Ischemic Stroke (TRACK) stent-retriever thrombectomy registry. Presented at: SNIS 13th Annual Meeting. July 25, 2016. Boston, MA.
Disclosures:
- Drs. Frei and Chen report no relevant conflicts of interest.
- Dr. Zaidat reports being a primary investigator for the TRACK registry, for which his institution received funding.