Key Points:
- Study explores association between admission BP, early outcomes after endovascular stroke therapy
- Patients with higher systolic BP tend to have poorer functional outcome at 3 months
Patients with acute ischemic stroke who have a higher systolic blood pressure (BP) at the time of hospital admission for endovascular therapy tend to have poorer functional outcome 3 months later, according to an observational study published online May 4, 2016, ahead of print in the Journal of NeuroInterventional Surgery.
Nitin Goyal, MD, of the University of Tennessee Health Sciences Center (Memphis, TN), and colleagues prospectively evaluated 116 consecutive patients with acute ischemic stroke with emergent large vessel occlusion who presented to a tertiary stroke center during a 4-year period. All underwent endovascular therapy.
“Prior studies have shown that high admission BP levels have been associated with lower recanalization rates after endovascular treatment for emergent large vessel occlusion strokes,” Dr. Goyal told Neurovascular Exchange via email.
Patients’ mean age was 63 years. At the time of admission, their median NIHSS score was 17 and median final infarct volume was 30 cm3.
Systolic BP and diastolic BP were measured using automated cuff recordings. Higher admission systolic BP correlated with larger final infarct volume (P = .020). Patients with a favorable functional outcome at 3 months, defined as an mRS 0-2, had lower admission systolic BP than those with poorer outcomes (151 ± 24 mm Hg vs 165 ± 28 mm Hg, P = .010), while admission systolic BP levels were higher in patients who died during hospitalization than in those who did not (169 ± 34 mm Hg vs 156 ± 24 mm Hg, P = .043).
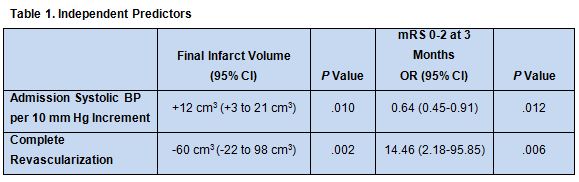
In linear regression models that adjusted for numerous potential confounders—including demographics; vascular risk factors; diastolic BP, NIHSS score, and serum blood glucose at admission; IV thrombolysis; onset to groin time; collateral score; and successful revascularization—each 10 mm Hg increment in admission systolic BP was independently associated with a larger final infarct volume and lower likelihood of favorable functional outcome at 3 months. The only other independent predictor of these outcomes was complete revascularization, defined as TICI IIb-III (table 1).
According to Goyal et al, the findings “should be cautiously interpreted, since excessive BP lowering in patients with ELVO prior to revascularization may reduce cerebral blood flow with the risk of exacerbating cerebral hypoperfusion and increasing ischemic injury. Consequently, our findings underline the importance of BP monitoring before, during, and after revascularization in order to avoid both excessively high and low BP levels.”
Seby John, MD, of the Cleveland Clinic (Cleveland, OH), was similarly circumspect about how to interpret the results. “In the setting of a large vessel occlusion, a higher baseline BP could be a compensatory response to maintain cerebral blood flow to the ischemic penumbra,” he wrote in an email to Neurovascular Exchange. “As such, aggressive early BP control before the vessel is recanalized could further decrease blood flow to affected areas, thus potentially carrying the risk of increasing infarct.”
Dr. Goyal agreed this is a possibility, although he pointed out there are several mechanisms through which BP may be related to recanalization and outcomes. “Experimental and clinical studies have demonstrated that higher BP increases blood brain permeability and cerebral edema in the immediate post stroke period,” he said. “Early cerebral swelling may increase resistance to residual blood flow and impair the recanalization process, leading to worse outcomes. On the other hand, it has been argued that cellular swelling is unlikely to develop within the first few hours of cerebral ischemia.”
Other possibilities, Dr. Goyal suggested, are that “greater thrombus burden in the occluded artery may lead to higher admission systolic BP levels, and thus the association between increased systolic BP levels and adverse outcomes may reflect the increased underlying clot burden.” Alternatively, he added, “higher admission systolic BP may lead to stronger hemodynamic force, resulting in higher impaction of the clot, thereby increasing the difficulty of mechanical retrieval.” He pointed out that Liebeskind et al have shown “a strong association between higher admission systolic BP levels and poorer degrees of collateral flow, which in turn were related to a lower likelihood of recanalization and functional independence.”
“At this time,” said Dr. John, “we do not have a standard BP target range for patient undergoing endovascular therapy. Extreme arterial hypertension or hypotension is clearly deleterious to multiple organ systems, but there is likely a BP range that is optimum for maintaining cerebral perfusion for each individual during an ischemic stroke. However, there is limited scientific evidence for such a target range now.”
Based on current evidence, he said, “in patients with large vessel occlusion, BP should be rigorously monitored before, during, and after undergoing endovascular therapy. We need prospective randomized trials of BP treatment after recanalization therapy (either IV tPA or endovascular therapy) that should be stratified according to absence or presence of recanalization. We also need prospective studies that will assess the natural history of BP in the setting of interventional therapies.”
Source:
Goyal N, Tsivgoulis G, Iftikhar S, et al. Admission systolic blood pressure and outcomes in large vessel occlusion strokes treated with endovascular treatment. J NeuroInterv Surg. 2016;Epub ahead of print.
Disclosures:
Drs. Goyal and John report no relevant conflicts of interest.