Key Points:
- Study explores contrast-induced acute kidney injury in stroke patients undergoing cerebrovascular angiography
- Proteinuria was the strongest independent predictor of kidney damage
The presence of proteinuria is by far the strongest independent predictor that stroke patients undergoing cerebral angiography will experience contrast-induced acute kidney injury (AKI), according to research published online April 22, 2016, ahead of print in the Journal of NeuroInterventional Surgery.
Investigators led by Li Zhang, MD, and Xinling Liang, MD, of Guangdong General Hospital (Guangzhou, China), retrospectively analyzed data on 2,015 patients who underwent cerebral angiography for stroke between January 2009 and December 2013.
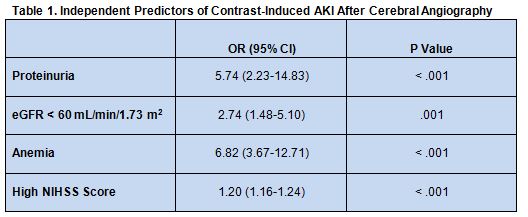
Overall, 85 patients (4.2%) were identified as having contrast-induced AKI. After adjusting for potential confounding risk factors, proteinuria (defined as urine dipstick trace to 3+ protein based on routine urine analysis or a urine albumin–creatinine ratio > 30 mg/g) emerged as the primary independent risk factor for developing the condition, although additional risk factors were also identified (table 1)
The presence of proteinuria was not associated with increased in-hospital mortality (OR 1.25; 95% CI 0.49-3.17; P = .639), but it was linked with greater likelihood of dying by 1 year (HR 2.30, 95% CI 1.55-3.41, P < .001).
Need to Test for Proteinuria Remains Unclear
In an email to WLNCMD, Perry Ng, MD, of Centura Health Physician Group (Denver, CO) explained that the most commonly identified risk factor for contrast-induced nephropathy is stage III chronic kidney disease, defined as an estimated glomerular filtration rate (eGFR) less than 60 mL/min/1.73 m2 for more than 3 months. “It is therefore not surprising that patients with pre-existing proteinuria had a higher incidence of contrast-induced nephropathy” in this study, he said.
The pathogenesis for contrast-induced kidney damage is similar for both cerebral and coronary angiography, said Dr. Ng, but it is typically both rare and self-limiting with regard to cerebral angiography. “I have never had a patient develop acute renal failure requiring dialysis in over 15 years of doing thousands of cerebral angiograms,” he said. “Most likely the higher incidence in the coronary literature of 1-2% in the general population and up to 50% in high-risk subgroups is related to the higher incidence of comorbidities such as advanced age, diabetes, heart failure, etc in patients requiring percutaneous coronary intervention.”
What remains unclear in this study, he noted, is whether patients with proteinuria were given renal protection via prehydration. “We are only told that 24.7% with contrast-induced nephropathy and 30.1% without contrast-induced nephropathy were given hydration therapy consisting of IV isotonic saline or sodium bicarbonate infusions,” he explained. “Patients with pre-existing renal impairment as identified by a creatinine > 1.3mg/dL or eGFR< 60ml/min/1.73m2 are those who would benefit most from prehydration before contrast administration.”
As noted by the authors, “proteinuria itself may exacerbate renal injury and make the kidney less tolerant of nephrotoxic insults such as contrast media,” added Dr. Ng. “This has not been proven to my knowledge, and neither the American College of Radiology Manual on Contrast Media nor the European Society of Urogenital Radiology Consensus Working Panel have promoted routine testing for proteinuria prior to contrast administration to date.”
While the current “study implies that all patients undergoing cerebral angiography for stroke should have routine testing for proteinuria beforehand,” he continued, “I’m not sure I believe it enough to incorporate into my clinical practice.”
According to Dr. Ng, “established guidelines to reduce contrast-induced nephropathy include performing iodinated contrast studies only when clinically necessary, minimizing the contrast volume injected, use of low or iso-osmolar contrast media, and renal protection protocols for patients with elevated creatinine/eGFR.”
Renal protection may consist of “isotonic saline or sodium bicarbonate infusions commencing 1hour before and continued for 6 hours after angiography,” he added. “N-acetylcysteine was previously proposed to reduce contrast-induced nephropathy but has been shown subsequently to not be efficacious. Due to its low side effect profile, some providers still use it.”
Source:
- Tao Y, Dong W, Li Z, et al. Proteinuria as an independent risk factor for contrast-induced acute kidney injury and mortality in patients with stroke undergoing cerebral angiography. J NeuroIntervent Surg. 2016;Epub ahead of print.
Disclosures:
- The study authors and Dr. Ng report no relevant conflicts of interest.