Key Points:
- Survey evaluates changes in care of acute stroke after publication of 5 seminal clinical trials showing benefits of mechanical thrombectomy
- Mechanical thrombectomy is being used more frequently
 Neurointerventionalists have responded to the recent clinical trial evidence in favor of mechanical thrombectomy for acute ischemic strokes caused by large-vessel occlusions by increasingly adopting this strategy, according to an informal survey. The findings were reported online April 21, 2016, ahead of print in the Journal of NeuroInterventional Surgery.
Neurointerventionalists have responded to the recent clinical trial evidence in favor of mechanical thrombectomy for acute ischemic strokes caused by large-vessel occlusions by increasingly adopting this strategy, according to an informal survey. The findings were reported online April 21, 2016, ahead of print in the Journal of NeuroInterventional Surgery.
Kyle M. Fargen, MD, of the Medical University of South Carolina (Charleston, SC), and colleagues asked Society of NeuroInterventional Surgery (SNIS) physicians to complete a 21-question online survey that addressed how their practices from before January 1, 2015, to the months following.
“We had noticed increased enthusiasm for mechanical thrombectomy with increased procedural volumes at our home institutions, both among neurointerventionists and stroke neurologists, after the publication of the New England Journal of Medicine randomized trials [ie, Goyal et al, Saver at al, Campbell et al, Berkhemer et al, and Jovin et al.],” Dr. Fargen told WLNCMD in an email. “We performed this survey to understand if these were pervasive trends throughout the United States.”
Overall, 78 physicians responded, representing about 10% of the SNIS membership. The physicians reported that the number of thrombectomies performed on a monthly basis at their institutions increased substantially after January 1, 2015 (table 1). In addition, 45% reported performing more thrombectomies after publication of the 5 trials.
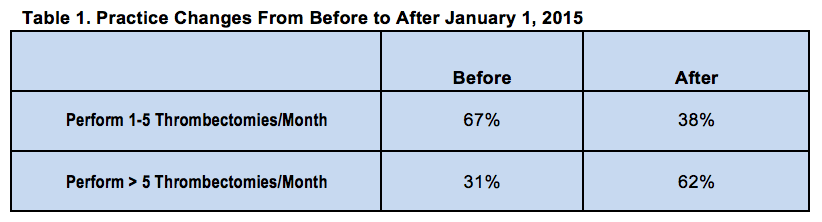
In addition, 73% of respondents reported that inpatient consultations for thrombectomy increased, and 80% said that hospital-to-hospital transfers for thrombectomy increased after January 1, 2015.
In terms of the procedure itself, 40% of respondents reported using A Direct Aspiration First Pass Technique (ADAPT) as the first strategy for revascularization. Nearly three-quarters of physicians said they were successful with their primary technique in at least 70% of cases. Conscious sedation was used for most of the procedures (56%).
Physicians Respond to the Evidence
In a telephone interview with WLNCMD, Philip Meyers, MD, of NewYork-Presbyterian Hospital and Columbia University Medical Center (New York, NY), pointed out that given the nonscientific nature of the survey it is impossible to discount the possibility of bias. The survey did, however, include the opinions of active interventionalists from both academic and private practices across the United States. He said he suspects that the findings are likely an accurate indication of practice trends, and they do reflect his own experience and observations.
“The good news is it shows that physicians do respond to scientific publications and scientific evidence,” he said, pointing out that in addition to the 5 key clinical trials demonstrating the benefits of mechanical thrombectomy, several meta-analyses, including his own, have confirmed the findings. Taken together, he said, it is appropriate that mechnical thrombectomy for eligible patients with emergent large-vessel occlusions has become the standard of care.
Dr. Fargen reached a similar conclusion. “This is a perfect example of the evolution of patient care based on high-quality evidence,” he said. “Consider the history of thrombectomy for emergent large-vessel occlusions and the evolution of thrombectomy device design, starting with intraarterial pro-urokinase to MERCI to retrievable stents. Consider the refinement in patient selection techniques, as exemplified by the limitations of the 3 randomized trials published in 2013, which helped to shape the requirements for enrollment in the recent positive trials. Now is an exciting time because finally the evidence supports the intervention, but by no means is the research or device innovation going to stop.”
The only really surprising finding, according to Dr. Fargen, was identification of ADAPT as the most common thrombectomy technique. “This is particularly interesting because the published randomized trials almost exclusively utilized retrievable stent technology,” he said. “This is reflected in the American Heart Association/American Stroke Association guidelines, which state that a retrievable stent should be used. It is therefore interesting that many physicians have moved on to a different first-line technique for thrombectomy in only a short period of time since these trials and guidelines have been published.”
Patient Selection Still Under Investigation
Identifying appropriate patients remains an important goal of research. “Many centers are pushing the envelope when it comes to selection criteria,” said Dr. Fargen. “The same evidence doesn’t exist for certain patients because the merits of thrombectomy have not been studied in a rigorous fashion in patients with certain occlusion locations, symptom severities, imaging profiles, or longer time course from symptom onset. In these cases, we have to choose patients carefully and make informed decisions regarding the risks and benefits of thrombectomy.”
Dr. Meyers noted that a much wider population of patients may actually benefit from mechanical thrombectomy than has been identified to date. “It’s now a fairly select group among all patients with acute stroke,” he said. “About 40% of acute strokes are due to large-artery occlusions, the target group for intervention. We are treating only a small portion. Probably, there are many more patients who may be candiates.” Trials designed to answer this question are ongoing.
Source:
- Fargen KM, Arthur AS, Spiotta AM, et al. A survey of neurointerventionalists on thrombectomy practices for emergent large vessel occlusions. J NeuroInterv Surg. 2016;Epub ahead of print.
Disclosures:
- Dr. Fargen reports no relevant conflicts of interest.
- Dr. Meyers reports being second past president of the SNIS.

