Key Points:
- Study addresses blood pressure changes following intra-arterial therapy for acute ischemic stroke
- Systolic blood pressure drops more in recanalized than nonrecanalized patients
A drop in blood pressure (BP) following cerebral artery recanalization in patients with acute ischemic stroke may be a sign of successful recanalization, according to research published online April 15, 2016, in the Journal of NeuroInterventional Surgery. But the window during which BP manipulation may produce clinical benefit could be more narrow than expected.
Seby John, MD, of the Cleveland Clinic (Cleveland, OH), and colleagues performed a retrospective analysis of 62 patients with acute ischemic stroke who underwent intra-arterial therapy for occlusion of the internal carotid artery terminus (22.5%), M1 middle cerebral artery (74.2%), or both (3.2%) between January 2008 and February 2012.
Overall, 59.7% achieved successful recanalization, defined as TICI 2b–3.
To exclude the effect of general anesthesia on BP, Dr. John explained in a telephone interview with WLNCMD, the researchers included only patients who underwent mechanical thrombectomy with IV sedation and without endotracheal intubation.
Patients who achieved successful recanalization had a higher baseline CT ASPECTS score (mean 8.3 vs 7.4; P = .046), a higher rate of IV tissue plasminogen activator (tPA) administration (51.5% vs 20.8%; P = .014), and higher rates of good outcome, defined as an mRS score of 0-2 (32.3% vs 9.5%; P = .045).
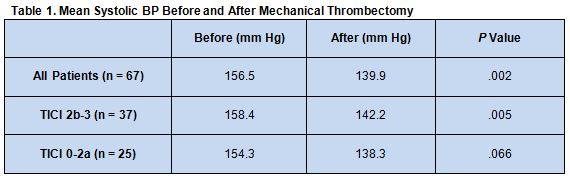
There were no differences between patients with vs without successful recanalization in systolic BP values measured before and after thrombectomy. Systolic BP at the end of the procedure, however, was lower than that measured before thrombectomy in the overall cohort; this difference was significant among patients with—but not among those without—successful recanalization (table 1).
Measurements of hourly changes in systolic BP over the following 36 hours revealed a greater fall occurring among successfully recanalized patients compared with those without successful recanalization. This difference was only significant, however, from 8 to 12 hours postprocedure. After this time, systolic BP decreased further in the nonrecanalized group to match that of those with successful recanalization. Systolic BP variation through 36 hours was similar in the 2 groups.
Marker of Recanalization
“We’ve confirmed [previous] results that a decline in blood pressure happens once you open the artery up,” said Dr. John. This series is unique from previous studies, however, in that it looked at patients who underwent mechanical thrombectomy (as opposed to IV tPA alone) and monitored systolic BP changes hourly for a full 36 hours.
Dr. John speculated that the BP changes observed “are just a reflection of the body’s endogenous drive to increase blood pressure [in order] to increase cerebral perfusion [in the face of] an occluded cerebral artery . . . . Once the artery is opened up, that can decrease, and the response is lower blood pressure.”
If this is the case, then a drop in systolic BP can be used as a marker of successful recanalization, he said, pointing to a paper published last month showing that lower [systolic] BP predicts good outcomes after endovascular therapy for acute stroke. “Extrapolating from both studies, I think if you see a significant blood pressure drop and clinical improvement, it suggests that the artery is recanalized,” he said.
But it appears that the key blood-pressure differences between occluded and nonoccluded patients only last about 12 to 14 hours, said Dr. John. That means that efforts to augment blood pressure in patients who are not recanalized are likely only to be beneficial during this narrow time window. “That is the new finding of this study,” he said, “and the implications may be extrapolated to patients given IV tPA also.”
He said considerably more research needs to be done on the relationship between blood pressure and ischemic stroke. It still remains unclear which blood pressure parameters are most clinically relevant, what they really mean, and how they can be modified to improve patient outcomes.
Source:
- John S, Hazaa W, Uchino K, Hussain MS. Timeline of blood pressure changes after intra-arterial therapy for acute ischemic stroke based on recanalization status. J NeuroInterv Surg. 2016;Epub ahead of print.
Disclosures:
- Dr. John reports no relevant conflicts of interest.