Key Points:
- Study seeks out factors influencing outcomes after successful recanalization with mechanical thrombectomy
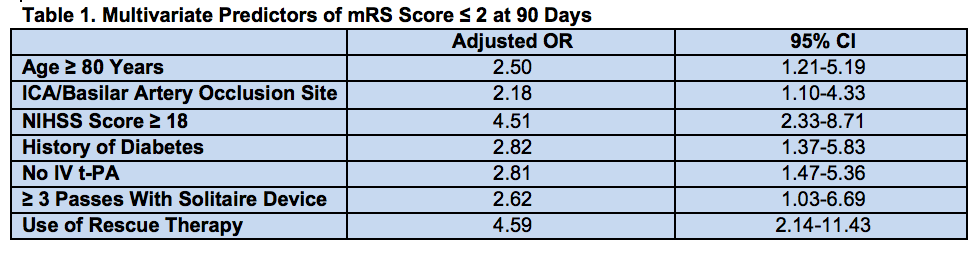
- Multiple predictors include patient age, occlusion site, NIHSS score, use of rescue therapy
 A new analysis of registry data has identified multiple patient- and treatment-related factors that foretell the functional outcomes of acute stroke patients after successful recanalization with mechanical thrombectomy. The findings were published in the March 2016 issue of the Journal of NeuroInterventional Surgery.
A new analysis of registry data has identified multiple patient- and treatment-related factors that foretell the functional outcomes of acute stroke patients after successful recanalization with mechanical thrombectomy. The findings were published in the March 2016 issue of the Journal of NeuroInterventional Surgery.
Older age, occlusion site, National Institute of Health Stroke Scale (NIHSS) score, and use of rescue therapy all were independent predictors of 90-day modified Rankin Scale (mRS) score 0-2.
Investigators led by Italo Linfante, MD, of Baptist Hospital (Miami, FL, used data from the North American Solitaire Stent Retriever Acute Stroke (NASA) registry to look at 354 patients treated with the Solitaire (Covidien) device.
Among them, 72.3% were had successful recanalization, defined as a Thrombolysis in Cerebral Infarction (TICI) score ≥ 2b. Of the 234 recanalized patients whose mRS score was ascertained at 90 days, 49.6% had poor outcomes.
Univariate analysis found multiple predictors of poor functional outcome (P ≤ 0.05), including older age, occlusion site, and high NIHSS score.
Multivariate analysis revealed a similar list of independent predictors of poor outcome at 90 days in a model with “good predictive power,” the study reports (c-index = 0.80; table 1).
While recanalization has been shown to be a powerful predictor of outcomes in acute ischemic stroke, “with the current technology and logistics, unfavorable outcomes (mRS ≥ 3) occur in 49% of patients despite successful recanalization,” the researchers point out, adding, “It remains important to understand which factors influence poor outcomes despite adequate recanalization.”
Of the predictive factors they identified, “the strongest effects were NIHSS score and rescue therapy,” they write, “both of which increased the risk of a poor outcome approximately fourfold whereas the increase estimated for each of the other factors was 2-3.”
Given that most of the predictors are not modifiable, they conclude that “[r]educing delays in reperfusion … may be the best way to improve clinical outcomes and should be considered in clinical trials that evaluate [intra-arterial] thrombectomy.”
Source:
- Linfante I, Starosciak AK, Walker GR, et al. Predictors of poor outcome despite recanalization: a multiple regression analysis of the NASA registry. J NeuroInterv Surg. 2016;8:224-229.
Disclosures:
- The study authors report no relevant conflicts of interest.

