Key Points:
· Medicare data used to assess link between physician/hospital experience, CAS outcomes
· Less experience tied to higher 30-day mortality
Physicians and hospitals that are more experienced at performing carotid artery stenting (CAS) achieve lower 30-day mortality rates than those that are less familiar with the procedure, according to research published online October 30, 2015 in Circulation: Cardiovascular Quality and Outcomes.
Investigators led by Soko Setoguchi, MD, of the Duke Clinical Research Institute (Durham, NC), linked Medicare claims to the 2005–2009 Centers for Medicare and Medicaid Services’ CAS Database in order to explore the relationship experience and outcomes.
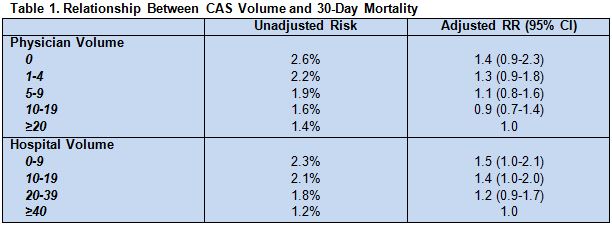
Overall, the unadjusted 30-day mortality risk was 1.8% among 19,724 patients (mean age 76.3 years; 60.1% men) who underwent CAS by 2,045 physicians in 729 hospitals.
Most patients (91.2%) were deemed to be at high surgical risk, and 47.4% were symptomatic, with a mean degree of carotid stenosis of 85.1%.
Three in 10 patients were treated by physicians who had performed fewer than 5 CAS procedures in the previous year, and 23.9% were treated by an operator with a past-year CAS volume of at least 20 cases. Two in 10 patients received CAS at centers where fewer than 10 cases were done in the past year, and 26.1% were treated at centers with at least 40 CAS procedures.
Greater physician experience with CAS was associated with lower 30-day mortality risk for patients, as was greater hospital experience (both P for trend < .05; table 1).
At a hospital level, coronary and peripheral artery stenting volume also was inversely tied to patients’ 30-day mortality risk after CAS (P for trend < .05).
Patient Selection Also a Factor
Periprocedural mortality rates reported here are higher than those reported in landmark clinical trials, including SAPPHIRE and CREST. The authors suggest this discrepancy may be explained by patient selection in addition to physician/provider experience.
“The median volume of CAS in Medicare patients for physicians was 9 per year and for hospitals was 23 per year,” Setoguchi told WLNCMD in an email. “One of the factors keeping the volume relatively low compared to carotid endarterectomy is that physicians from various subspecialties (eg, cardiology, vascular surgery, radiology, and interventional neurology) can perform the CAS procedure.”
“Many patients are treated by low-volume physicians, and high-volume providers tend to select healthier patients,” he continued. “Therefore, periodic monitoring of periprocedural complications after CAS can help in assessing the appropriateness of patient selection and in updating training and proficiency requirements for CAS providers, as necessary.”
Source:
Jalbert JJ, Gerhard-Herman MD, Nguyen LL, et al. Relationship between physician and hospital procedure volume and mortality after carotid artery stenting among Medicare Beneficiaries. Circ Cardiovasc Qual Outcomes 2015;Epub ahead of print.
Disclosures:
- Setoguchi reports no relevant conflicts of interest