Observational data on nearly 12,000 cases show that 30-day death/stroke risk is reduced for patients receiving CAS after surgery or as a repeat procedure.
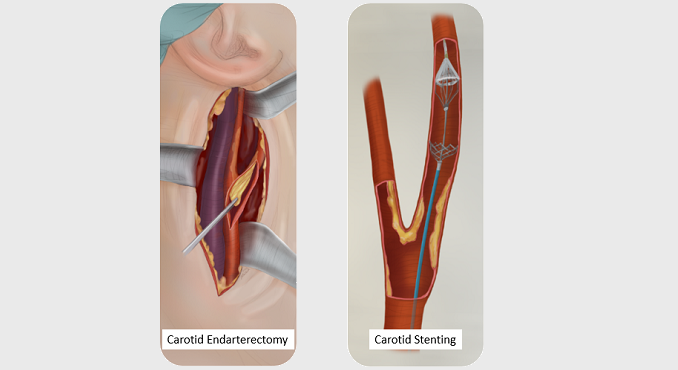
Symptomatic patients who are undergoing carotid artery stenting (CAS) either as a redo procedure or after prior ipsilateral carotid endarterectomy (CEA) have a lower composite stroke/death risk at 30 days than those receiving primary CAS. Moreover, these procedures are associated with less bradycardia and hypotension but more hypertension, observational data show.
“Restenosis is a recognized complication of carotid revascularization,” say investigators led by Isibor J. Arhuidese, MD, MPH (Johns Hopkins Medical Institutions, Baltimore, MD). In the CREST trial, they point out, rates reached 9.7% for CEA and 12.2% for CAS at 10 years, with restenosis linked to a fourfold increase in stroke risk.
“Hence, the need for reintervention in patients with hemodynamically significant disease,” the researchers observe, adding, “Little is known of the outcomes of CAS performed on the background of prior carotid intervention relative to CAS performed for primary disease.”
As outlined in their paper recently published in Stroke, Arhuidese and colleagues retrospectively analyzed outcomes from the Vascular Quality Initiative, which is a prospectively maintained database of the Society for Vascular Surgery. In all, there were 11,742 CAS cases performed between 2003 and 2016—72% were primary procedures, 5% repeat CAS, and 23% CAS after prior ipsilateral CEA. Most patients were being treated for asymptomatic disease and ipsilateral stenosis > 80%.
At 30 days, stroke/death rates were similar across the three groups when looking at asymptomatic patients. But among symptomatic patients, the rate was lowest for those undergoing CAS after CEA, with an odds ratio of 0.60 (95% CI 0.37-0.98) when compared with those undergoing primary stenting. By 1 year, the likelihood of stroke/death no longer differed.
Stroke/Death Rates at 30 Days After CAS
|
|
Primary |
Post-CEA |
Post-CAS |
P Value |
|
Asymptomatic |
2.5% |
2.0% |
1.3% |
0.23 |
|
Symptomatic |
5.2% |
2.6% |
5.0% |
0.003 |
Predictors of stroke/death at 30 days were urgent/emergent procedures and placement of two stents in the post-CEA group, whereas in the redo-CAS group, they were older age, male sex, symptomatic status, American Society of Anesthesiologists class IV status, and urgent/emergent procedures.
Bradycardia was less common in patients undergoing CAS either after CEA (OR 0.32; 95% CI 0.26-0.39) or as a redo procedure (OR 0.55; 95% CI 0.39-0.78) compared with those receiving primary CAS. The same was true for hypotension requiring IV treatment, both for the post-CEA (OR 0.41; 95% CI 0.35-0.48) and redo-CAS groups (OR 0.66; 95% CI 0.50-0.86). However, hypertension requiring IV treatment was more common among patients undergoing CAS after CEA (OR 1.66; 95% CI 1.43-1.94) or as a repeat procedure (OR 1.55; 95% CI 1.18-2.05).
“Our results show that CAS is not without risks in all groups of patients studied,” Arhuidese et al observe. They go on to describe the differences in heart rate and blood pressure seen here despite adjustment for preoperative medication use as “remarkable,” noting that the “effect of angioplasty and stenting on the carotid reflex and the physiological adaptations over time are well known.”
Given that hemodynamic disturbances have been linked by the International Carotid Stenting Study and others to periprocedural stroke, clinicians should “anticipate and mitigate these hemodynamic events as they occur, in line with the ongoing aim to further lower the procedural risk associated with carotid revascularization,” the investigators advise. Some centers have suggested that prophylactic atropine might prevent intraoperative bradycardia and cardiac morbidity during CAS, they add, but data are slim and require validation at a population level.
Overall, the predictors of adverse events found here “underscore the importance of preprocedural risk assessment, anticipation, prompt recognition, and rescue of at-risk patients,” Arhuidese and colleagues conclude. “Adequate planning ensures that optimal human and material resources are available to intervene at the earliest sign of a potential adverse event in a timely manner. Consequently, the benefits of planned procedures cannot be overstated.”
Sources:
Arhuidese IJ, Rizwan M, Nejim B, Malas M. Outcomes of primary and secondary carotid artery stenting. Stroke. 2017;Epub ahead of print.
Disclosures:
Arhuidese reports no relevant conflicts of interest.

