Key Points:
- Retrospective study evaluates whether the 2010 release of CREST data affected type of carotid revascularization
- Proportion of CAS vs CEA held steady between 2009, 2011
Release of data from CREST in 2010 did not sway clinicians towards one way or the other toward stenting vs surgery for the treatment of carotid artery disease, according to a study published online July 21, 2015, ahead of print in Neurosurgery.
|
Implications
Influence of CREST may still be seen in “the next 2 or 3 years,” study author says.
|
CREST, more formally known as the Carotid Revascularization Endarterectomy vs. Stenting Trial, generated controversy when first published in 2010 in the New England Journal of Medicine for not decisively clarifying whether carotid artery stenting (CAS) or carotid endarterectomy (CEA) is best for patients with symptomatic or asymptomatic carotid stenosis.
The trial showed no difference in the composite of stroke, MI, and death at 4 years, though in the periprocedural period, stroke was more common with stenting and MI more frequent with surgery.
To evaluate CREST’s effects on clinical practice, Farhan Siddiq, MD, of Thomas Jefferson University (Philadelphia, PA), and colleagues compared National Inpatient Sample data on 225,191 patients (mean age 70.9 years; 58.2% men) who underwent CAS or CEA in 2009 and 2011.
Baseline characteristics differed between groups. Before CREST, patients undergoing CAS were more likely to have congestive heart failure, CAD, and renal failure than those receiving CEA. After CREST, the same baseline differences existed, with the addition of a higher prevalence of A-fib in the CAS group.
More Neurological Complications for Stented Patients
Among carotid revascularization procedures, the proportion that were CAS did not change between 2009 and 2011 (12.3% vs 12.7%; P = .90).
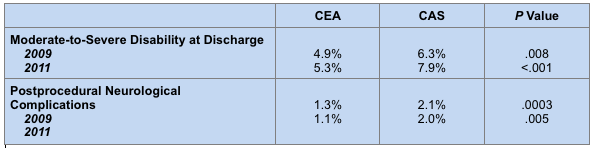
In-hospital complication rates were similar between the 2 treatment types during both the pre- and post-CREST periods. Patients receiving CAS in 2009 and 2011 were more likely than those who underwent CEA in the same years to be discharged with moderate-to-severe disability and to have postprocedural neurological complications (table 1).
Table 1. Unadjusted Outcomes Before vs After CREST Publication
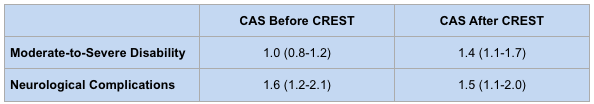
Multivariate adjustment was performed to account for differences in age, sex, and risk factors, with CEA in the pre-CREST era serving as the reference group. After adjustment, CAS patients only showed an increased risk of moderate-to-severe disability compared with CEA patients when treated after CREST’s publication. However, the higher likelihood of neurological complications for CAS patients remained apparent in both 2009 and 2011 (table 2).
Table 2. Risk of Adverse Outcomes vs Pre-CREST CEA: Adjusted OR (95% CI)
Overall, these findings suggest that “the CREST results have not made a significant impact on the current practice patterns and outcomes in the United States,” the study authors say, although they acknowledge that their short, 1-year windows may have limited their ability to detect changes in trends in clinical practice.
Noteworthy is that “[p]eriprocedural neurological complications, including stroke and intracerebral hemorrhage, continued to be more frequent in the CAS group in pre- and post-CREST eras,” the investigators write. That discrepancy is consistent with the CREST finding of a “slightly higher” risk of postprocedural stroke with CAS vs CEA, which may have led clinicians to continue favoring surgery, they posit.
Changes Coming to Carotid Revascularization
However, Dr. Siddiq told WLNCMD in a telephone interview that although CAS may be slow to gain traction, clinicians should start to see the impact of CREST within “the next 2 or 3 years.” In the meantime, his group expects to continue reviewing patient data up to 2014.
Given that many clinicians are trained to perform either CAS or CEA—but not both—the biggest impact of CREST will “come from physicians who can do both procedures because they have a better understanding of which procedure has a better outcome in every clinical scenario,” Dr. Siddiq explained.
Nonetheless, one major hurdle for the proliferation of CAS will be getting clinicians onboard with performing the procedure, Dr. Siddiq said. “Reimbursement is a factor because Medicare currently only reimburses for [CAS] only in instances where CEA is high risk.” Other Medicare requirements are stenosis severity of at least 70% and ipsilateral cerebral ischemic symptoms.
Yet Dr. Siddiq sees a future for CAS, noting that the 2014 American Heart Association/American Stroke Association guidelines “for stroke treatment have definitely recommended [CAS] as a reasonable alternative to [CEA]. So I think that’s a major step.”
Source:
Siddiq F, Adil MM, Malik AA, et al. Effect of carotid revascularization endarterectomy versus stenting trial results on the performance of carotid artery stent placement and carotid endarterectomy in the United States. Neurosurgery. 2015;0:1-7.
Disclosures:
Dr. Siddiq reports no relevant conflicts of interest.
Related Stories:
No Advantage for CAS Patients Enrolled in CREST at Later Dates

