Key Points:
- Analysis assesses changes in carotid stenting, surgery outcomes over 8 years of enrollment in CREST
- Periprocedural outcomes with CAS held steady, even with adjustment for potential confounders
Despite better patient selection and increasing experience with carotid artery stenting (CAS) over the course of the Carotid Revascularization Endarterectomy versus Stenting Trial (CREST), there were no concurrent improvements in periprocedural events over time. The findings come from a new analysis published online July 14, 2015, ahead of print in Stroke.
CREST generated controversy when first published in 2010 in the New England Journal of Medicine for not decisively clarifying whether CAS or carotid endarterectomy (CEA) is best for patients with symptomatic or asymptomatic carotid stenosis. The trial showed no difference in the composite of stroke, MI, and death at 4 years. Periprocedurally, stroke was more common with stenting and MI more frequent with surgery.
Period 1: January 2001 through January 3, 2006 (n = 832)For the current study, Thomas G. Brott, MD, of the Mayo Clinic (Jacksonville, FL), and colleagues examined whether periprocedural outcomes remained consistent for CAS over time. They divided the 2,502 patients randomized in CREST according to 3 periods of enrollment:
- Period 2: January 4, 2006, through March 19, 2007 (n = 839)
- Period 3: March 20, 2007, through July 2008 (n = 831)
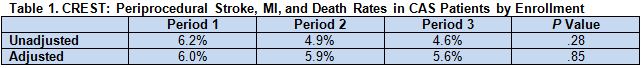
Within the CAS cohort, crude rates of the combined endpoint of periprocedural stroke, MI, and death were similar regardless of when patients were randomized. Patients gradually became younger on average and more likely to be men, lack symptoms, and have dyslipidemia over the 3 enrollment periods; adjustment for these 4 factors provided a similar result (table 1).
Calculations that took into account the level of operator experience at participating sites also failed to show any differences among enrollment periods for the CAS group.
Further analysis showed a trend toward improvement in the composite endpoint for asymptomatic CAS patients (unadjusted rates of 4.6% vs 3.6% vs 3.0% for periods 1, 2, and 3, respectively; P for trend = .44) that was not demonstrated in symptomatic CAS patients. The same patterns were seen for the combined endpoint of stroke or death and when rates were adjusted for age, sex, and dyslipidemia.
Among patients randomized to CEA, the rate of the composite outcome decreased between periods 1 and 2 before increasing in period 3.
Data Do Not Settle Debate
Study coauthor George Howard, DrPH, of the University of Alabama at Birmingham (Birmingham, AL), however, stressed to WLNCMD in an email that the results must be interpreted cautiously. Namely, he stated, there is no guarantee that CAS outcomes remained the same; the only thing that can be said is that no evidence of change was observed.
“Admittedly, the study was not designed to well describe changes over time, but this is the largest study of CAS versus CEA, and if these large changes were occurring, CREST offered the best opportunity to see these changes,” Dr. Howard explained.
One contributor to the steady outcomes is the low CAS event rates, which did not leave much room for improvement over the study period, he said, adding that the lack of change reflects highly on the study investigators, “who very carefully picked out the [CAS] operators to have a high skill level at the beginning of the study.”
According to Christopher J. White, MD, of Ochsner Medical Center (New Orleans, LA), the heterogeneity of the CREST data—which opens the door to confounding—“seriously compromises” the investigators’ ability to detect temporal differences. For example, the analysis did not account for operator volume, he pointed out.
“These data are not convincing to me, and I do not believe they will impact the opinion of the trial,” he told WLNCMD in an email interview, expressing surprise that there was no sign of decline in CAS complications.
Dr. White asserted that CREST does not speak to today’s CAS outcomes. “If we repeated CREST today, we would get better outcomes,” he commented. “The newer equipment; smaller, more flexible embolic protection devices; proximal protection devices; and easier-to-deliver stents would contribute to fewer complications.”
Much work is being done to improve CAS, Dr. Howard agreed. He expressed hope that the efforts are successful but said “it is going to be hard to prove the new devices are working better, as this is going to require studies with very large sample sizes.”
CREST-2 stands out as the best chance to make the case, Dr. Howard reported.
Source:
Howard G, Hopkins LN, Moore WS, et al. Temporal changes in periprocedural events in the Carotid Revascularization Endarterectomy versus Stenting Trial. Stroke. 2015;Epub ahead of print.
Disclosures:
· Drs. Brott, Howard, and White report no relevant conflicts of interest.