Key Points:
- Researchers look at endovascular management of carotid, vertebral artery dissection
- Treatment is safe, reduces risk of recurrent stroke; characteristics differ by dissection type
Endovascular management of cervical dissection is safe and effective, according to a single-center, restrospective analysis published online September 23, 2016, ahead of print in the Journal of NeuroInterventional Surgery. The authors maintain, however, that medical management remains the recommended first-line option.
Felipe C Albuquerque, MD, of St Joseph’s Hospital and Medical Center (Phoenix, AZ), and colleagues conducted a retrospective analysis of their prospectively maintained institutional database. They identified 116 patients (mean age 44.9 years) with extracranial dissection who underwent endovascular intervention between 1996 and 2016.
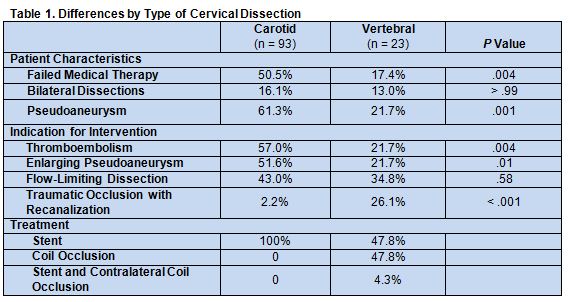
Of these patients, 93 had dissections of the carotid artery and 23 of the veretebral artery. Treatment included 104 stent placements, 11 coil occlusions of the patent artery, and 1 stenting with contralateral vessel occlusion.
Patients with carotid vs vertebral artery dissection were well-matched for age, sex, dissection etiology, and admission and follow-up mRS scores.
Patients with carotid artery dissections were more likely than patients with vertebral artery dissections to require endovascular intervention as a result of enlarging pseudoaneurysms or thromboembolic events. They were also more likely to fail medical therapy and be treated with a stent. In contrast, patients with vertebral artery dissections were more likely to require endovascular intervention for traumatic occlusion with recanalization (table 1).
Dissections were spontaneous in 67 patients, traumatic in 36, and iatrogenic in 13. Patients with carotid artery dissections that were caused by trauma had lower admission mRS scores (P = .01). Six of the 67 patients with spontaneous dissection (9.0%) reported having a recent chiropractic manipulation.
During a mean follow-up period of 3.5 years (range 1-146 months), permanent morbidity or mortality occurred in 3.4% of patients, including two deaths. Over a follow-up period of 364 patient-years, 1 stroke occurred, for an annual rate of 0.27%.
At last follow-up, 41 previously disabled patients—comprising 33.3% of those with a carotid artery dissection and 43.5% of those with a vertebral artery dissection—were no longer disabled. No patients reported worsened disability.
Medical Management Remains First-line Option
“This series is the largest reported to date of patients undergoing endovascular intervention for cervical dissection,” wrote the authors. “However, although patients undergoing only medical therapy were not analyzed for this study, we still advocate medical management as the first-line therapy for most patients with [carotid or vertebral artery dissection], and we do not wish to imply that the results of intervention are superior to those of medical management.”
Nonetheless, the authors concluded that “endovascular management of cervical dissection is highly effective in preventing recurrent stroke among patients with specific indications, and it has an acceptable complication profile.” It is important to recognize, they point out, that patients with carotid v. vertebral artery dissection “differ significantly in presentation, indications for treatment, and the most appropriate endovascular treatment methods.”
Source:
Moon K, Albuquerque FC, Cole T, et al. Stroke prevention by endovascular treatment of carotid and vertebral artery dissections. J NeuroInterv Surg. 2016;Epub ahead of print.
Disclosures:
Dr. Albuquerque reports no relevant conflicts of interest.