Key Points:
- Registry trial compares long-term outcomes of CEA vs CAS for stroke prevention
- Risk of ipsilateral stroke, death at median of 4 years higher with stenting
A Swedish analysis of registry data has uncovered a considerably greater long-term risk of stroke and death for patients treated with carotid artery stenting (CAS) versus carotid endarterectomy (CEA) for stroke prevention.
However, Christopher White, MD, of the Ochsner Medical Center (New Orleans, LA), told Neurovascular Exchange that interpretation of the findings is limited by a number of methodological flaws in the study. He said he remains unconvinced by the data, noting that far different results have already been reported in better designed, more robust randomized controlled trials.
Magnus Jonsson, MD, of the Karolinska Institute (Stockholm, Sweden), and colleagues looked at long-term outcomes among 1,157 patients registered in the national Swedish Vascular Registry (Swedvasc) who had undergone CAS (n = 409) or CEA (n = 748) between 2002 and 2012 for prevention of stroke.
Every patient who underwent stenting was matched with 2 patients who underwent endarterectomy based on sex, age, procedure year, and indication (symtomatic/asymtomatic). Postoperative stroke was identified by cross-matching the cohort with the InPatient Registry and charts review.
Approximately three-quarters of patients were male, mean age was 70 years, and 69% were symptomatic. Risk factor profile was similar between the 2 groups.
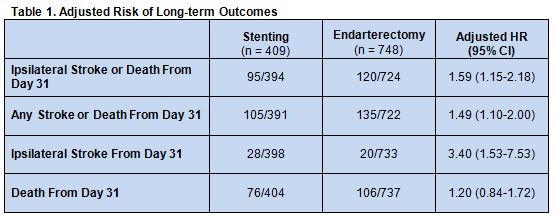
During a median follow-up time of 4.1 years, the primary endpoint of ipsilateral stroke or death > 30 days after intervention occurred more frequently in patients who underwent CAS compared with CEA. Similarly, the risk of any stroke or death > 30 days after intervention and the risks of ipsilateral stroke alone or death alone during this time period all were more common among CAS-treated patients.
After adjusting for confounders that included smoking, pulmonary disease, diabetes, hypertension, heart disease, renal disease, and atrial fibrillation, risks of all of the above outcomes—except for death alone, which no longer was statistically significant—continued to be increased with CAS (table 1).
Highlighting what he sees as the study’s limitations, Dr. White explained that it does not address how patients were selected for either treatment. “This is critical, because it can be a strong bias favoring CEA if only healthy subjects are chosen for surgery,” he said. “A high percentage of patients (60%) in the registry were symptomatic from their carotids, while only 50% were symptomatic in CREST [and] 100% were in ICSS.”
Nor does the paper include information on the qualifications of the operators or on procedural volume, Dr. White added. “This is ‘administrative data’ taken from coded charts rather than clinical information that is audited in a clinical trial like CREST or ICSS. The data is also ‘self-reported,’ meaning if the surgeon does nto report the stroke, or write it in the chart, it never happened.”
Additionally, some of the data reported were quite surprising, Dr. White noted. “It describes a very high (30%) stroke and death event rate favoring CEA, which is much higher than the concurrent randomized trials, CREST or ICSS.” The long-term mortality rate for stenting also seemed unusualy high and the rate of ipsilateral stroke unusually low, he said.
In their paper, the researchers acknowledge many of the same study limitations, though they stress numerous strengths, among them the use of a nationwide database to assess real-world outcomes and the large sample size.
“This nationwide cohort study shows that CAS confers an increased long-term risk of stroke and death when compared to CEA,” they conclude. “This increased risk is mainly explained by an increased rate of ipsilateral stroke after the periprocedural period, indicating that CAS is not as durable as CEA for treatment of carotid artery stenosis.”
Source:
Jonsson M, Lindström D, Gillgren P, et al. Long-term outcome after carotid artery stenting: a population-based matched cohort study. Stroke. 2016;Epub ahead of print.
Disclosures:
- Dr. Jonsson reports no relevant conflicts of interest
- The study was partly funded by the Swedvasc registry
- Dr. White reports being a member of the Interventional Management Committee of the CREST-2 Trial, sponsored by the National Institutes of Health