Though there are now alternatives, introduction of Onyx was “revolutionary,” one expert says.
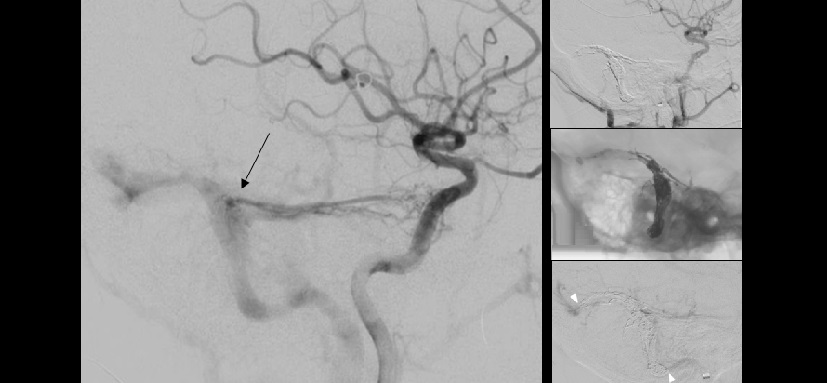
Treating intracranial dural arteriovenous fistulas (dAVFs) using the dimethyl-sulfoxide (DMSO)-based Onyx liquid embolization system results in good initial and midterm outcomes, according to data from single-center registry analysis and meta-analysis.
The findings were published online recently ahead of print in Neurosurgery.
Alejandro Berenstein, MD (Mount Sinai Hospital, New York, NY), commenting on the study for Neurovascular Exchange, said that Onyx (EV3, Irvine, CA) has become the standard of care for dAVFs. Other DMSO-based liquid embolic treatments are available elsewhere in the world for the treatment of dAVFs and arteriovenous malformations, including Squid (Emboflu) and PHIL (MicroVention Terumo).
Currently only Onyx is approved for use in the United States, however. Its availability represented a revolution in the treatment of dAVFs, he explained, because previously treatment necessitated sacrificing the sinus. “Onyx permits in multiple cases to preserve the sinus,” he said.
The authors, led by Benjamin Gory, MD, PhD (Normandie University, Caen, France), analyzed data from their prospectively maintained registry of 33 consecutive patients with 36 dAVFs who were treated with 41 transarterial embolizations using Onyx. They also conducted a systematic review of all 19 studies examining outcomes of transarterial embolization using Onyx, for a total of 425 patients with 463 dAVFs.
In the prospective study, complete occlusion was achieved in 32 of 36 fistulas (88.9%). Of the 31 fistulas that were followed-up, four recurred (12.9%). Two dAVFs were retreated. Procedure-related morbidity was 3%, and there were no procedure-related deaths.
A meta-analysis of both the registry findings and the literature data revealed somewhat lower complete occlusion and recurrence rates and similar morbidity and mortality rates. There was “significant heterogeneity” across studies for occlusion rate but not for the other endpoints.
Pooled Outcomes of Onyx
|
|
Rate (95% CI) |
|
Initial Complete Occlusion |
82% (74%-88%) |
|
Midterm Recurrence |
2% (0-5%) |
|
Postoperative Neurological Deficit |
4% (2-6%) |
|
Procedure-Related Morbidity |
3% (1-5%) |
|
Procedure-Related Mortality |
0 |
According to Berenstein, these are good outcomes for dAVF. At his center, morbidity rates are approximately 0.5% and total occlusion occurs in about 90% of patients, he reported.
Improvements Continue
“Some of the advantages of the newer agents, such as PHIL, are that they are made radiopaque with iodine, whereas the Onyx is made radiopaque with tantalum,” explained Berenstein. “The ability to see through the embolic agent is better when it’s iodine. But the Onyx introduction was a leapfrog advancement. The introduction of PHIL and Squid are [just] improvements on the same platform. The Onyx introduction was revolutionary.”
Still, said Berenstein, the long-term durability of Onyx-based repair has yet to be evaluated.
In comments published along with the study, Paul Foreman, MD, and Mark Harrigan, MD (Birmingham, AL), describe the findings as “favorable” and say that they have come to regard endovascular therapy as their first-line approach for intracranial dAVFs. They note, however, that the findings are limited by a lack of surgical comparison group (understandable given how few dAVFs are currently being managed in this manner) and possible publication bias.
“This report will serve as a contemporary summary of the risks and benefits of endovascular treatment of intracranial dAVFs for informed consent with patients prior to endovascular treatment,” they write. But they question its utility for clinical decision-making because of the lack of a surgical comparison group. It also provides no direct comparison to treatment using n-BCA-based liquid embolic systems, which the commentators themselves prefer.
A newer advance in the treatment of dural fistulas, said Berenstein, is investigation into the combination of DMSO-based agents with intra-sinus balloons, which protect the sinus while the embolic agent is being injected.
Source:
Sadeh-Gonike U, Magand N, Armoiry X, et al. Transarterial Onyx embolization of intracranial dural fistulas: A prospective cohort, systematic review, and meta-analysis. Neurosurgery. 2017;Epub ahead of print.
Disclosures:
- Gory and the commentators report no relevant conflicts of interest.
- Berenstein reports involvement in the development of the PHIL liquid embolic agent.