Key Points:
- Study prospectively tracks platelet inhibition during stenting for intracranial aneurysm
- Thromboembolic complications more frequent in patients with less adequate inhibition
Inadequate platelet inhibition is common among patients undergoing stenting for the treatment of intracranial aneurysm and is associated with an increased risk of thromboembolic complications, according to a paper published online November 20, 2015, ahead of print in the Journal of Neurosurgery.
The authors report that thromboelastography (TEG) can help identify these patients, so that their antiplatelet therapy protocol can be adjusted.
For the prospective analysis, investigators led by Youxiang Li, MD, PhD, of the Beijing Neurosurgical Institute and Beijing Tiantan Hospital (Beijing, China), followed 168 patients with intracranial aneurysms undergoing stent implantation. Diffusion-weighted MRI was performed within 24 hours of stenting to identify acute ischemic lesions, and TEG was used to assess the degree of platelet inhibition in response to clopidogrel and aspirin.
Mean maximal amplitude (MA) value was 63.4 mm. One-third of patients (34.5%) were resistant to clopidogrel, and the mean preoperative ADP inhibition was 27.5%. One in 5 patients was resistant to aspirin, with a mean arachidonic acid inhibition of 77.8%.
Overall, 91 patients (54.2%) had acute cerebral ischemic lesions. Six patients experienced perioperative TIA and 3 showed signs of permanent disability at discharge (5.4% in all), and 11 (6.5%) had thromboembolic complications during a mean follow-up period of 7.8 ± 2.3 months.
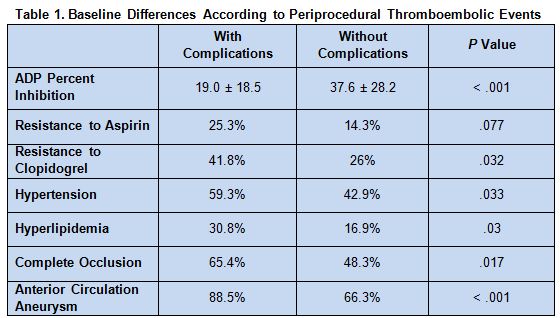
Patients with periprocedural thromboembolic complications were more likely to have lower percent adenosine diphosphate (ADP) percent inhibition, resistance to antiplatelet agents, hypertension, hyperlipidemia, complete occlusion, and aneurysm of the anterior circulation (table 1).
Independent risk factors for periprocedural complications were location in the anterior circulation (adjusted OR 4.17; 95% CI 1.65-10.53; P = .003) and ADP percent inhibition (adjusted OR 1.03; 95% CI 0.59–1.79; P < .001).
During follow-up, thromboembolic events were independently predicted by MA (adjusted OR 0.842; 95% CI 0.68-0.98; P = .038) and MA-ADP (adjusted OR 0.763; 95% CI 0.59-0.97; P = .022).
Balancing Risks
“The antiplatelet therapy protocol of patients with insufficient inhibition should be adjusted to decrease the risk of thromboembolic complications, and TEG can be used to adjust the antiplatelet therapy protocol of aneurysm patients undergoing stent treatment,” Dr. Li told WLNCMD in an email.
“Patients with insufficient platelet inhibition have a higher risk of thromboembolic complications,” he continued, noting that even so, many patients do not receive enough antiplatelet therapy. “Because we were not sure of the relationship of platelet inhibition and thromboembolic complications at the beginning of our study, we did not change the protocol of antiplatelet therapy” for clopidogrel-resistant patients, Dr. Li noted.
He explained that providing adequate antiplatelet therapy can be a challenge because there is no known “safe range” of platelet inhibition, in which the risks of thromboembolic and bleeding complications are both low. Currently, the research team is trying to pinpoint this range, Dr. Li reported.
Source:
Yang H, Li Y, Jiang Y. Insufficient platelet inhibition and thromboembolic complications in patients with intracranial aneurysms after stent placement. J Neurosurg. 2015;Epub ahead of print.
Disclosure:
- Dr. Li reports no relevant conflicts of interest.