Fusiform shape and use of three or more devices each were associated with higher risk of neurological complications with the flow diverter.
The Pipeline flow diverter can be safely used to treat selected aneurysms located in the posterior circulation, according to a recent large registry trial. Provided that aneurysms are not fusiform in nature, complication rates are no higher than those seen with clipping or coiling.
An out expert pointed out to NVX, however, that this registry looked at safety only, so the overall efficacy in terms of aneurysms occlusion was not addressed.
The Pipeline embolization device (PED; Medtronic) was originally approved for use in the anterior circulation, Christoph J. Griessenauer, MD (Harvard Medical School, Boston, MA), observed. As experience with the device and other flow diverters has grown, it is becoming increasingly clear that its potential utility is wider.
“Up until this study,” he explained, “there were mainly case series or single center case reports on the use of the Pipeline in posterior fossa. This is the first larger study.”
Given the rarity of these lesions, and Pipeline’s infrequent use for this indication, Griessenauer said, “Most centers just have a handful of cases. So, to have a large study like this provides a better picture of what the true risk is.”
For the study published online on September 27, 2017, ahead of print in Neurosurgery, Demetrius K. Lopes, MD (Rush University Medical Center, Chicago, IL), and colleagues conducted a subgroup analysis of IntrePED, a multicenter, single-arm, retrospective study conducted between July 2008 and February 2013 in 6 countries at 17 centers. The goal of the registry was to identify neurological complications that occur with use of the Pipeline device for the treatment of intracranial aneurysms in a real-world setting.
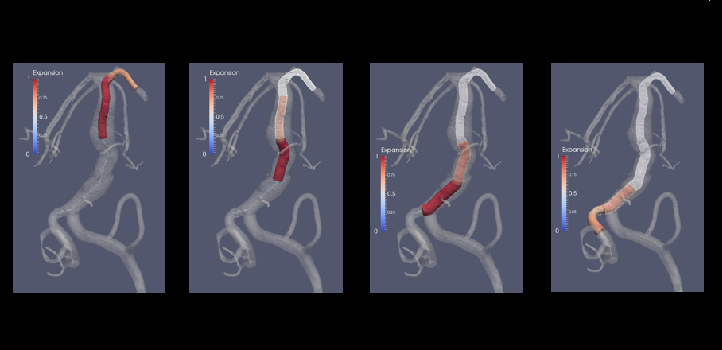
This subanalysis focused on 91 consecutive patients treated for 95 aneurysms occurring exclusively in the posterior circulation. Mean aneurysm size was 13.8 mm, and aneurysm types were saccular (36.8%), fusiform (29.5%), dissecting (28.4%), or other (5.3%). Patients were followed-up for a median of 21.1 months.
Overall, 12 patients experienced the primary outcome of a neurological complication leading to morbidity or death. Multivariate analysis revealed that the risk of this outcome was increased among patients who had three or more Pipeline devices implanted and when the aneurysms were of fusiform shape.
Predictors of Neurological Complications Causing Morbidity or Death
|
|
Hazard Ratio (95% CI) |
P Value |
|
Use of ≥ 3 Pipeline Devices |
7.77 (2.48-25.86) |
0.0007 |
|
Fusiform vs Any Other Aneurysm Shape |
3.48 (1.06-13.39) |
0.0488 |
In addition, there was an increased risk of neurological morbidity with treatment of aneurysms of increasing size (HR 1.11; 95% CI 1.04-1.18; P = 0.0015) as well as a higher risk of neurological mortality associated with ruptured aneurysms (HR 8.1; 95% CI 1.31-41.26; P = 0.0197) and advancing age (HR 1.07; 95% CI 1.02-1.15; P = 0.0262).
On univariate analysis, basial artery aneurysms were associated with an increased risk for major outcomes (HR 3.54; 95% CI 1.12-14.18; P = 0.0529).
Flow Diversion Could Meet Clinical Need
Griessenauer emphasized that there is currently no standard treatment for certain aneurysms of the posterior circulation. They have traditionally been treated with open surgery, which is both complex and associated with mixed outcomes. While clipping and coiling are options, these treatments have their own limitations, he said, suggesting that flow diverters such as the Pipeline could help fill a void.
According to the researchers, Pipeline “may be considered for the treatment of posterior circulation aneurysms, especially of saccular or dissecting type.
“Our major complications appear to be comparable to those reported previously after clipping and coiling in the literature,” they conclude. “Neurointerventionists should consider the shape, size, rupture, and location of complex posterior circulation aneurysms as well as age and PED number before the PED placement.”
Griessenauer agreed. “For dissecting and saccular aneurysms, the Pipeline device is probably very suitable,” he said. “For fusiform aneurysms, flow diversion does not necessarily present the ideal solution. But I think we are on the verge of expanding the indications for flow diversion in the posterior circulation.”
Another important finding of the study, he said, is that outcomes are generally best when as few devices as possible are used, much like when Pipeline is employed for aneurysms in the anterior circulation.
Unanswered questions remain. Use of flow diversion in the posterior circulation continues to be associated with a greater complication risk than in the anterior circulation, said Griessenauer, “possibly because the basilar arteries have a large number of perforating arteries that come off the basilar trunk. When these are covered by a flow diverter, patients may not tolerate that as well potentially as in the anterior circulation.” In addition, it remains unclear how to best treat large fusiform aneurysms in the posterior circulation.
He also pointed out limitations to the study. The IntrePED registry did not include complete information on clinical outcomes. Notably, it did not collect information on aneurysm occlusion rates (ie, angiographic outcomes), as it was designed to assess safety-related outcomes only. “Without information on aneurysm obliteration after Pipeline placement, the paper is of limited value, as aneurysm occlusion is the main purpose of Pipeline embolization,” he explained.
Source:
Lopes DK, Jang DK, Cekirge S, et al. Morbidity and mortality in patients with posterior circulation aneurysms treated with the pipeline embolization device: A subgroup analysis of the international retrospective study of the Pipeline Embolization Device. Neurosurgery. 2017;Epub ahead of print.
Disclosures:
- This study was funded by Medtronic.
- Lopes reports being a consultant for Covidien, Stryker, and Penumbra and being on the advisory board of Siemens Medical Solutions.
- Griessenauer reports no relevant conflicts of interest.