With good critical care management, patients likely fare as well or better with a short wait at the hospital for specialized personnel.
Hospitals considering whether to adopt a 24-hour “ultra-early” protocol for treating aneurysmal subarachnoid hemorrhage (SAH) might find some answers in data from a new analysis published online in the Journal of Neurosurgery. Specifically, the ultra-early approach is likely not necessary and could potentially do more harm than good, according to the single-center retrospective analysis.
“Most healthcare teams managing SAH patients have opted to treat ruptured aneurysms in an urgent fashion (within 12-24 hours) rather than ultra-early (immediately postadmission),” senior author Aditya S. Pandey, MD (University of Michigan, Ann Arbor, MI), explained to Neurovascular Exchange in an email. But “there was a recent publication outlining that ultra-early treatment could improve outcome by preventing a re-rupture, as may occur when we wait 12-24 hours.”
Pandey and his team hypothesized instead that, given recent improvements in critical care management, including better blood pressure and pain control, “the rate of rerupture while waiting for treatment is minimal, and thus changing the paradigm would not be worth the resource needs that would arise when changing to the ultra-early treatment paradigm.”
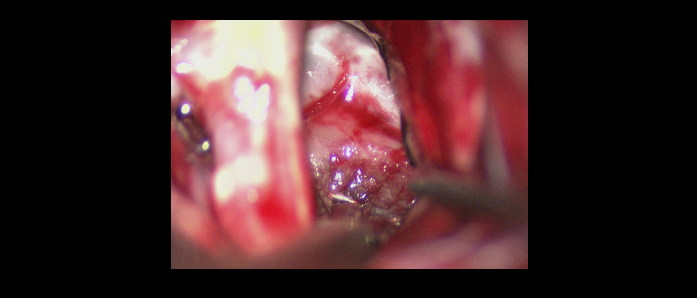
To test their hypothesis, the authors conducted a retrospective analysis of data from a prospectively collected cohort of 317 patients with aneurysmal subarachnoid hemorrhage. They defined rebleeding as new or expanded hemorrhage on CT, which was determined by independent review conducted by multiple physicians. The possibility that rebleeding might have been prevented by an ultra-early aneurysm repair via clipping or coiling was independently reviewed for each case of rebleeding.
Overall, only 24 of the 317 patients (7.6%, 95% CI 4.7-10.5) experienced rebleeding at any time point following initial aneurysm rupture. Of these, one patient (4.2%, 95% CI -3.8-12.2) was deemed to experience rebleeding that could have been prevented by ultra-early repair. Among the remaining 23 patients, rebleeding considered not to be preventable by an ultra-early approach because:
- It occurred prior to admission to the authors’ institution (14/23, 60.9%)
- The initial diagnostic angiography was negative for aneurysm (4/23, 17.4%)
- The rebleeding was postoperative (2/23, 8.7%)
- Patients were unable to undergo surgery due to medical instability (2/23, 8.7%)
- Rebleeding was intraoperative (1/23, 4.3%)
Ultra-Early Treatment Has Downsides
Pandey pointed out that adopting an ultra-early approach has its downsides. “There will be issues of allocating resources which would introduce greater costs and potential inefficiencies when managing elective cases,” he explained. “The clinical disadvantage would be that the ultra-early treatment may be provided by nursing and tech staff who do not participate in aneurysm treatment procedures on a daily basis.”
Lead author Joseph R. Linzey, BS (University of Michigan), added that they have recently demonstrated increased rates of complications among neurosurgery patients when the procedure is initiated after hours. “When a patient with an SAH presents overnight, not only do we save resources and staff by waiting to surgically treat the aneurysm in the morning, but theoretically, there is also a decreased risk of intra-operative or postoperative complications,” he explained to NVX.
Based on their findings, Pandey concluded that the current practice of providing early/urgent treatment is “safe, efficacious, and cost-effective, as it does not lead to a significant number of patients suffering from rerupture prior to treatment [so] long as there is good infrastructure for managing the critical care issues related to SAH.”
He did add, however, that larger collaborative studies are needed to confirm the results and determine whether they are generalizable to other centers.
Source:
Linzey JR, Williamson C, Rajajee V, et al. Twenty-four-hour emergency intervention versus early intervention in aneurysmal subarachnoid hemorrhage. J Neurosurg. 2017;Epub ahead of print.
Disclosures:
- Pandey reports receiving grants from the National Institutes of Health and the American Heart Association.
- Linzey reports no relevant conflicts of interest.

