Key Points:
- Meta-analysis compares internal trapping, stent-assisted coiling for vertebral artery dissecting aneurysms
- Both options have similar feasibility, outcomes, and risks
Both internal trapping and stent-assisted coiling are equally good options for the endovascular management of intradural vertebral artery dissecting aneurysms, according to a meta-analysis published online May 24, 2016, ahead of print in the Journal of NeuroInterventional Surgery. The study authors provide some guidance on which approach might be more appropriate in specific situations.
Hongqi Zhang, MD, of Xuanwu Hospital (Beijing, China), and colleagues report that intradural vertebral artery dissecting aneurysms have been identified as an important cause of both subarachnoid hemorrhage and ischemic stroke, thus warranting prompt attention.
“Given its minimally invasive characteristics, endovascular treatment of [intradural vertebral artery dissecting aneurysms] has become the dominant approach,” they write. “The two most commonly used methods are internal trapping and stent-assisted coiling, although selection of the ideal treatment remains controversial.”
Dr. Zhang and colleagues performed a meta-analysis of 8 retrospective studies testing these two options in 188 patients with intradural vertebral artery dissecting aneurysms.
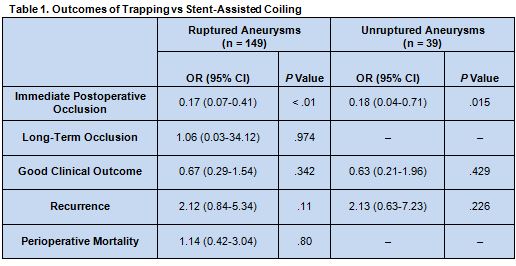
The immediate postoperative occlusion rate was greater for patients treated with trapping rather than stent-assisted coiling, no matter whether aneurysms were ruptured or unruptured. No differences were uncovered, however, for the outcomes of long-term occlusion, clinical outcome, recurrence, or perioperative mortality between the two treatment modalities (table 1). Notably, lack of data meant that long-term occlusion and perioperative mortality rates could not be calculated among patients with ruptured aneurysms.
Two Solid Options
“This meta-analysis showed that both internal trapping and stent-assisted coiling techniques are effective in the treatment of ruptured and unruptured [intradural vertebral artery dissecting aneurysms],” write the authors. They point out that both approaches are technically feasible, have high rates of good long-term neurologic outcomes as well as low recurrence and mortality rates, according to their analysis.
The authors note several limitations of their study, including its nonrandomized nature, lack of a validated classification system for intradural vertebral artery dissecting aneurysms, lack of a uniform assessment of complications, and some missing data, including no details at all on patients treated with flow diverters.
Regarding selection of a treatment modality for individual cases, “Overlapping stents and appropriate use of antiplatelets may decrease the risk of rebleeding and recurrence,” they advise. “For unruptured [intradural vertebral artery dissecting aneurysms], conservative treatment is recommended. For patients with enlarged aneurysms and those with progressive ischemia after medical management, both internal trapping and stent-assisted coiling are good choices. When the [posterior inferior cerebellar artery] origin is involved in a ruptured [intradural vertebral artery dissecting aneurysms], bypass surgery or [vertebral artery-to-posterior inferior cerebellar artery] stent placement plus coil embolization should be considered.”
Source:
Guan J, Li G, Kong X, et al. Endovascular treatment for ruptured and unruptured vertebral artery dissecting aneurysms: a meta-analysis. J NeuroInterv Surg. 2016;Epub ahead of print.
Disclosures:
Dr. Zhang reports no relevant conflicts of interest.