Key Points:
- Proof-of-concept study looks at accuracy of 3D printing in 4 pediatric patients (3 AVMs, 1 VOGM)
- Consistency established among structural measurements of real lesion, multiple models
Utilizing 3D printing technology can produce accurate models of intracranial vascular malformations in children that facilitate shorter operative time, according to a proof-of-concept study published online July 31, 2015, ahead of print in the Journal of Neurosurgery: Pediatrics.
“Treatment of complex neurovascular lesions… requires careful application of meticulous surgical and/or endovascular technique,” Edward Smith, MD, of Boston Children’s Hospital (Boston, MA), and colleagues write. “In particular, risk is especially elevated in children, who have smaller blood volumes, complicated anesthetic requirements, and more difficult surgical and endovascular access as compared with adults.”
The researchers used an in-house 3D print service to construct multiple models of 3 arteriovenous malformations (AVMs) and 1 vein of Galen malformation (VOGM) found in 4 pediatric patients. The printer (Connex 500; Stratasys), which can produce up to 2 resins simultaneously at a detail of 16 microns, was fed with data from several MRI and CT scans using specialized software.
Among open surgical cases, sizing fidelity was assessed by comparing intraoperative photographs with model photographs taken at the same angle. Anatomical structures were also measured intraoperatively and compared with the same structures on the models.
High Fidelity
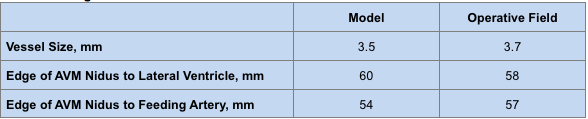
Less than 10% deviation was found among 5 areas in 3 surgical models. Overall, there was 98% agreement (range 94%-100%) in measurements in vessel size, distance from AVM to ventricle, and distance from outer edge of nidus to feeding artery (table 1).
Table 1. Average Measurements of Selected Anatomical Features of AVM Cases
The VOGM was successfully embolized without complication. Based on vessel angulation as seen on visual comparison of the right and left anterior cerebral arterial segments supplying the lesion, microcatheter navigation was used. “This assessment would have been extremely difficult to derive from 2D image displays, and the predicted ease of navigation was borne out during the embolization,” the authors write.
Resection was successful in all 3 AVM cases, with total angiographic obliteration confirmed by perioperative angiography. No transfusions were required and the only postoperative complications were an expected transient hemiparesis and sensory loss in the large right parietal lesion, both of which more or less resolved within 1 week.
Lastly, compared with “closely matched controls,” the use of 3D printed models “may potentially reduce operative time by approximately 12%,” the authors add.
Tangible Understanding
Simulation and specifically 3D printing, having proved successful in multiple other fields of medicine, are especially useful for clinicians treating children with neurovascular disease, Dr. Smith and colleagues say, because “the ability to employ multiple resins of varying consistency and color, coupled with submillimeter accuracy and production times measured in hours rather than weeks, has radically improved the verisimilitude of anatomical models.” A caveat, they add, is that the MRI sequences need to be provided in high resolution.
Emphasizing the limitations of their small study, the authors say they still see “essential value in the provision of an illustrative, proof-of-principle result… [F]urther study into costs and benefits for institutions beyond improving training and surgical outcomes may be warranted with a larger cohort of patients.”
Lastly, anecdotal evidence suggests a greater level of both physician and patient comfort in understanding lesion pathology and treatment implications, they conclude.
Source:
Weinstock P, Prabhu SP, Flynn K, et al. Optimizing cerebrovascular surgical and endovascular procedures in children via personalized 3D printing. J Neurosurg Pediatr. 2015;Epub ahead of print.
Disclosures:
- The study was supported by the Kids at Heart Neurosurgery Research Fund and the Lucas Warner AVM Research Fund.
- Dr. Smith reports no relevant conflicts of interest.