Key Points:
- Retrospective study examines outcomes with endovascular treatment of head, neck AVMs
- Cure or improvement were common, with a low risk of complications
Head and neck arteriovenous malformations (AVMs) present a rare and unique challenge. But a new study published online August 26, 2016, ahead of print in the Journal of NeuroInterventional Surgery suggests that, with careful technique, they can be managed safely.
Dan Meila, MD, of Sana Kliniken Duisburg (Duisburg,Germany) conducted a retrospective analysis of 14 patients treated endovascularly for the condition between 2000 and 2014 via a transarterial superselective microcatheter-based approach followed by embolization using liquid embolic agents.
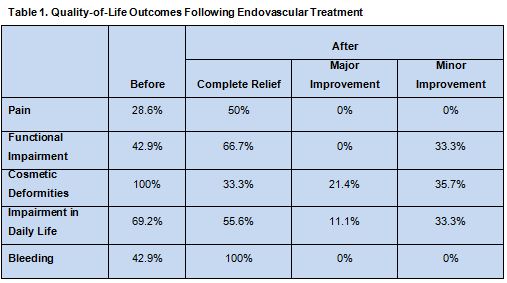
Patients completed quality-of-life questionnaires regarding the following symptoms before and after treatment: pain, functional impairment, cosmetic deformity, impairment in daily life, and bleeding.
Complete or > 90% closure of the AVM was achieved in 6 of 14 patients (43%), and > 50% shunt reduction was achieved in 10 patients (71%). During a total of 86 endovascular procedures, there were 6 complications.
Six patients presented with bleeding, which was cured in all cases. Pain was resolved in 2 of 4 patients. Functional
impairment was cured in 4 of 6 patients and improved in the other 2. Cosmetic concerns were present in all cases and improved in all but 2 patients. Impairment in daily life was lessened or resolved in 9 patients (table 1).
Multidisciplinary Team Is Essential
In a telephone interview with Neurovascular Exchange, Charles Prestigiacomo, MD, of Rutgers New Jersey Medical School (Newark, NJ) and president of the Society of NeuroInterventional Surgery, explained that head and neck AVMs represent an excessively rare and poorly understood pathology. “Treatment of these lesions is very difficult. It’s not often that we can completely cure them,” he said, adding, “It almost seems as if these AVMs can recruit more vessels over time. So, when you think you’ve shrunk an AVM or even potentially eradicated it, later it can come back.”
Dr. Prestigiacomo explained that endovascular treatment is usually an adjunct to more definitive surgical treatment, which can be both complex and risky. The main technical difference between treating a brain AVM and head and neck AVM, he said, is that the latter can be approached through direct puncture. “That has its own risks and certainly has its own experience base,” he noted.
Importantly, he said, head and neck AVMs should not be tackled by a single interventionalist. Rather, a multidisciplinary team is needed to determine which patients require treatment, how best to approach it, and to develop clear treatment goals.
Some head and neck AVMs are best left untouched, advised Dr. Prestigiacomo. “Some of these can be very deep under the skin, so they may present as just a bulge, but they are not in any way dangerous, and it might be [best] to just leave them alone.” He also stressed the importance of quality of life, saying, “If it is not a major cosmetic issue or if it is not actively bleeding, then you need to be very careful about embarking on treating this, because you can significantly alter quality of life and patient satisfaction.”
This study, noted Dr. Prestigiacomo, “shows that meticulous technique can lead to good results, but we need long-term follow-up.”
Regardless, using these techniques “without having a full team approach and a sense of what the treatment goals are before beginning the therapy is dangerous,” he concluded.
Source:
Meila D, Grieb D, Greling B, et al. Endovascular treatment of head and neck arteriovenous malformations: Long-term angiographic and quality of life results. J NeuroInterv Surg. 2016;Epub ahead of print.
Disclosures:
- Dr. Meila reports no relevant conflicts of interest
- Dr. Prestigiacomo reports being a consultant for education to Stryker, Codman, and Aesculap.